Spring is coming but it isn't here yet. Let's review the things you need to avoid/stop doing entirely if you want to have a healthy, pain-free back and neck this summer!! There are some things no back patient should ever do, but patients (and some soon-to-be patients) tend to try harmful activities every year anyway…So, how many are you guilty of? 1. Shovel snow. This is one of the toughest activities any home-owner ever takes on, but every spring we get one last blast that blocks the walk or driveway, and - all across the Mid-West - back patients reach for that shovel. If you've had recent back surgery, or you have a bad back for any reason, this is a job to avoid! Forever! And if you absolutely have to move some snow, do it like your feeding a chipmunk - little, tiny bites, handled gently. Snow is light when it's falling, but it gets very heavy when it hits the ground, particularly in spring when it tends to be wetter and denser. And that snow shovel is a big clumsy spoon, designed to pick up a lot of material at once. So each full shovel-full can easily exceed 20 lbs, which you're trying to pick up at an awkward angle while you're bending over, in the cold! It will only take three or four big heaves to strain your back muscles and send you into spasm, so take little 1/3 shovels full, move them by stepping, not throwing, or better yet, get some help! 2. Drive to Florida… Or embark on any long trip the week after back surgery or a recent back injury. Many of my patients travel a distance to have their surgery with me, and they have to get home that next week. The trip is safe and works out fine if
I've had a patient surreptitiously plan his post-op trip so he drove the family the whole way from Cleveland to South Beach 3 days after surgery! Then called to say he was really sore, his wound was red and swollen, and he had drainage on his unchanged bandage. Obviously there's nothing your local doctor can do for you at that point except shake his/her head! If you have to travel to get home after surgery, have a plan for someone to drive you or to accompany you on your flight. You can't be handling the luggage or running for a taxi. Even better, stay a few days in town and have a wound check before you make an extended trip by car or plane. And just don't decide you're still going to take that golf trip/cruise/motor home excursion just five days after your back or neck operation. Plan ahead and give it a little time! 3. Try moving “that rock”… This is the gardener’s favorite mistake. Sure….it looked like such a little rock… But that was before you started digging!!! Every gardener knows this, but - for some reason - lots of gardeners can't stop themselves even though they know better. Every little rock is just the top of a much bigger rock! It's probably a good idea to stay out of the garden for a couple of weeks after surgery or injury in any event, but I've had a number of patients that "just couldn't". So, if that describes you, you should at least follow a couple of rules. If you are recovering from any kind of fusion surgery for the neck or back, you may sit in your garden and enjoy it. And that's IT! If you've had a discectomy or decompression surgery you still need to take it easy for 3 - 6 weeks before you start doing anything very vigorous. And, if you've had previous surgery, or you've had a back or neck injury in the past, you need to use good, common sense:
4. Walking the dog(s) before you’re ready… Yes, you love your dogs and they LOVE you! They’re glad to have you home and can't wait to get out and go for their walk!!! But it doesn't matter if they are big or small, they’re going to try to kill you! The big ones will bolt and drag you across the yard, which is disastrous if you've just had anything like back, shoulder or knee surgery, and the little ones will wrap that leash around your feet and trip you, which is just as bad or worse. If you are recovering from a back or neck injury or from any kind of back, neck, or Orthopaedic surgery, be careful! Share the dog-walking chore with someone who can help you, or have someone else give them a walk ‘til you're good on your feet. 5. Hosting that big Holiday, Thanksgiving, or any kind of affair involving lots of food, decorations, and furniture arranging too soon after surgery! Like the driving to Florida thing, you need to give yourself a little time to recuperate! If you do have surgery around the time of a big important event, make sure everyone knows you are now the spectator, not the chef d'cuisine. Whether it's a family get-together, a wedding, or some other once in a life-time event, you will be much happier and the family will be much happier if you watch - or, at most, point to stuff for younger hands to carry - than if you aggravate your back or neck and end up miserable or worse. Remember, that turkey weighed between 20 - 30 lbs before it was stuffed, and those big crocks, pans, and kettles - they're heavy when they're full. If you're the only one that knows the recipe, that's fine, but you need to recruit good helpers any time you're trying to protect your back at the holidays. 6. Anything involving a horse, a motorcycle, or an ATV - Let's just say any non-standard form of transportation that you have to feed, hold upright, or try not to bounce out of or off of! If you've had a recent back or neck injury or you are less than 6 weeks out from surgery, this is a good time to groom the horse, rebuild the bike, or polish the ATV. And any attempt to cut corners and get back to riding before you are ready will result in back and neck pain and spasm, at the least. Getting back to riding and back on the trail will be most successful if you take it in stages, build your strength up first, and then go back to activity a bit at a time. And when it comes to horses you can love them, comb them, watch them. But no riding and no chores that’re measured in buckets, bales, or bags! I used to tell my post-op patients who were ready for normal, unrestricted activity that they could go back to "everything but rugby and rodeo!" and everyone would chuckle. Until one day when the young woman I was so happy with started to tear up and sniffle. I had just one question - "You're a Barrel racer aren't you?". "Yes sir" she replied tearfully. So we had a nice long talk about sports rehab, and conditioning, and muscle strengthening to get ready to go back to her sport. And I learned never to tease my patients who have horses! 7. Deciding a tall stack of books will make an excellent step-ladder. I've had a patient decide this was a sound strategy. And at the age of 80 you'd think anyone would know better. Any time you have any kind of idea like this, go sit down for a while until the impulse passes. Please!! 8. General Gardening. Of course – no bending, lifting, or twisting for 8 weeks after surgery! “But it’s spring and those roses won’t plant themselves!” Again, find a helper, pay the gardener a little more, or enjoy last year's garden for a second season. If you are going to be "the muscle" in your yard then remember - nothing for 3-6 weeks after surgery, no lifting over 20 lbs until 6 weeks after surgery AND permission from your surgeon, and work in short stints - 30 minutes at a time, with a little walk about and rest to make sure your back or neck isn't tightening up. And, please, if you do over-do it - ice, anti-inflammatories and rest are the only thing for it. You won't need to call your doctor just to say you chopped wood all weekend and now your back is sore! He/she won't be able to do anything but offer sympathy... 9. Anything involving a chainsaw, engine hoist, or a bungee cord. Does anyone actually need say this…? As with Holiday dinners, the person recovering from a recent back or neck injury, or recent back or neck surgery can watch heavy operations. You can even point to stuff for younger folks to do. You can display your wisdom and experience for all to marvel at. But don't try to pick up, twist, or torque anything that would make someone else grunt! 10. Losing your pain medications – Whether it's down the sink, down the toilet, off the front seat of the car – it doesn’t matter. Now-a-days you can’t just call in for a refill. Your pharmacist likely won’t refill it no matter what your doctor says, because - by law - they have to keep track of how many prescriptions you fill in how many days. And recently, it hasn't mattered if this is your first pain prescription in decades or one of a number you've gotten over the years, your pharmacist can simply refuse to refill your refill. So take care of those pain medications the way you really ought to - very carefully.…  As always…I want my patients to be active, and get back to full fitness and recreation when they've healed up. But that always means taking care of your back and using good common sense at home and at work!
I hope you find this discussion interesting and useful. If you have other questions that I can answer for you, please leave a comment below. And feel free to like and follow my Facebook page to find more content that you and others might find helpful!
0 Comments
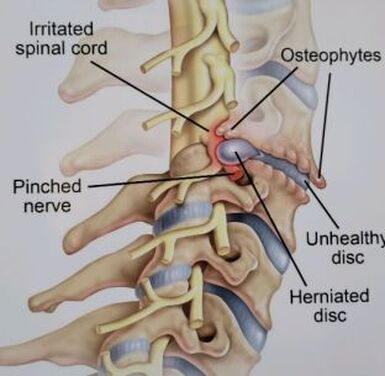
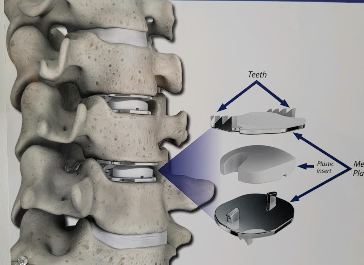
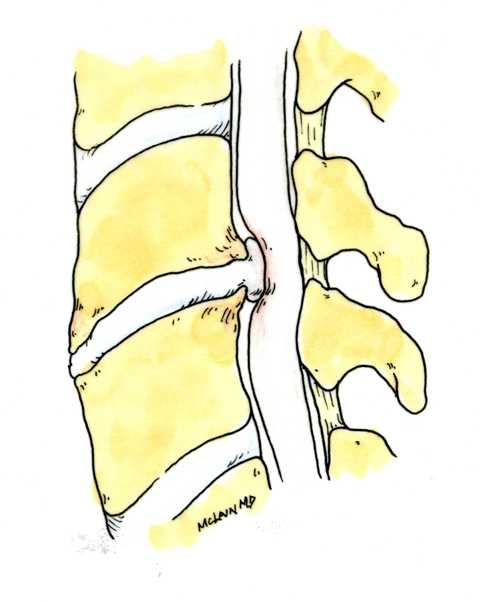
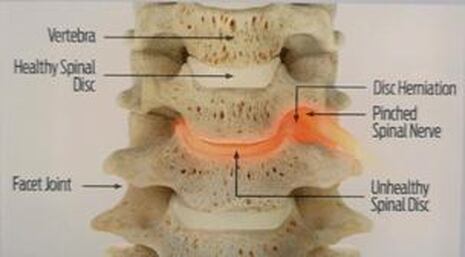
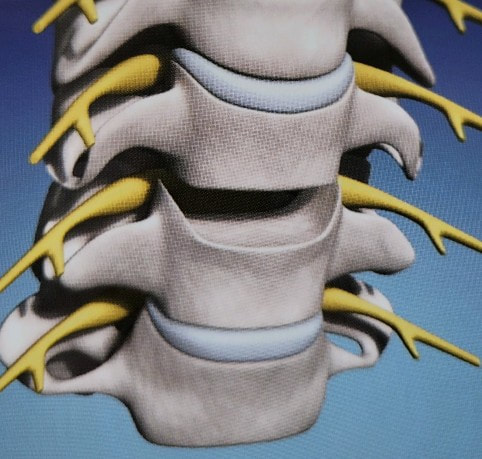
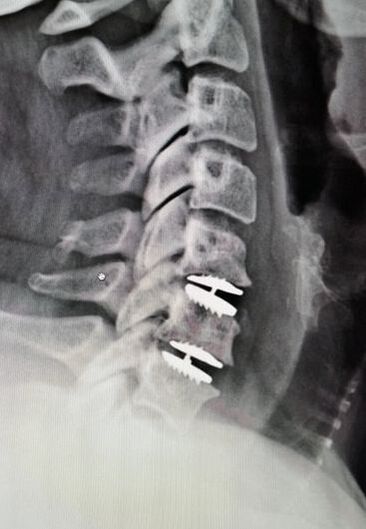
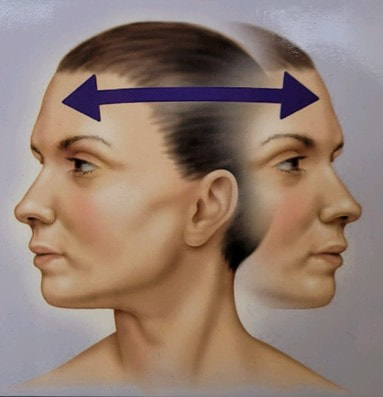
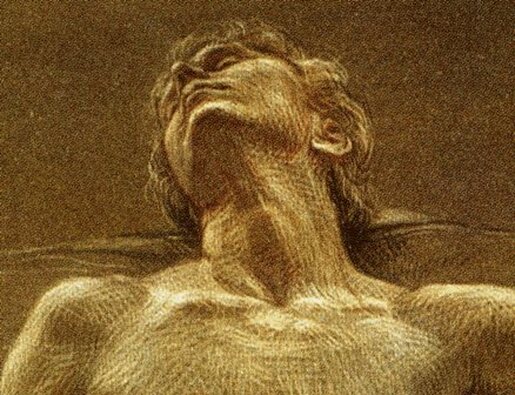
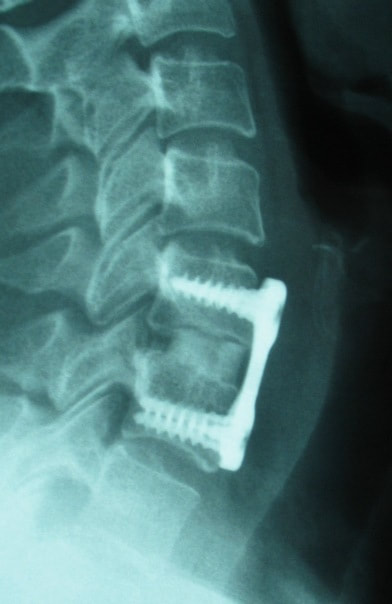
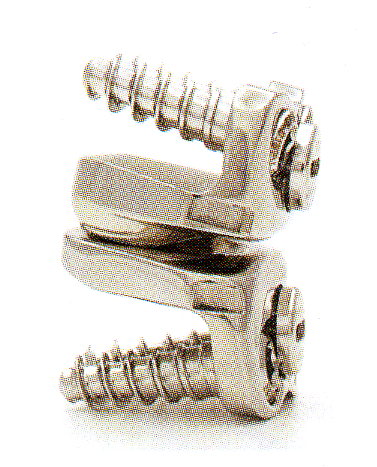
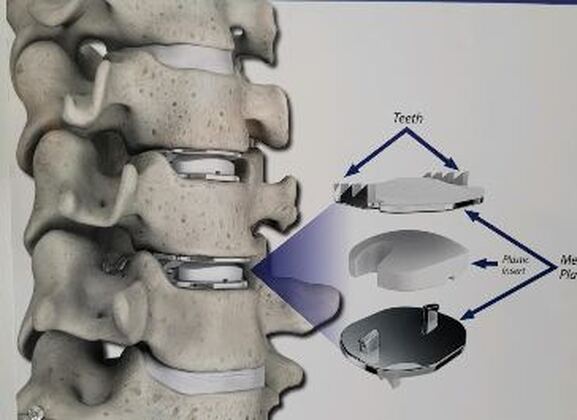
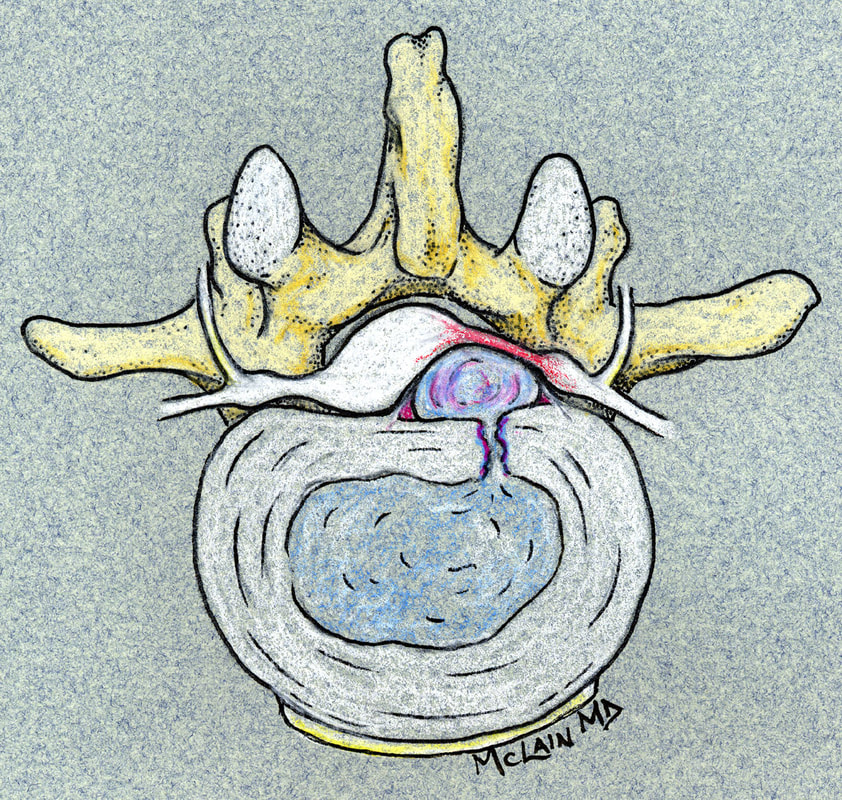
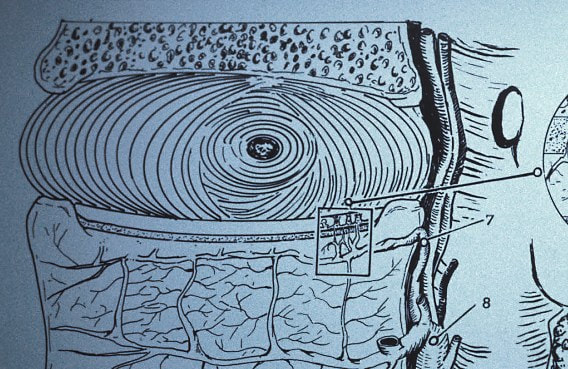
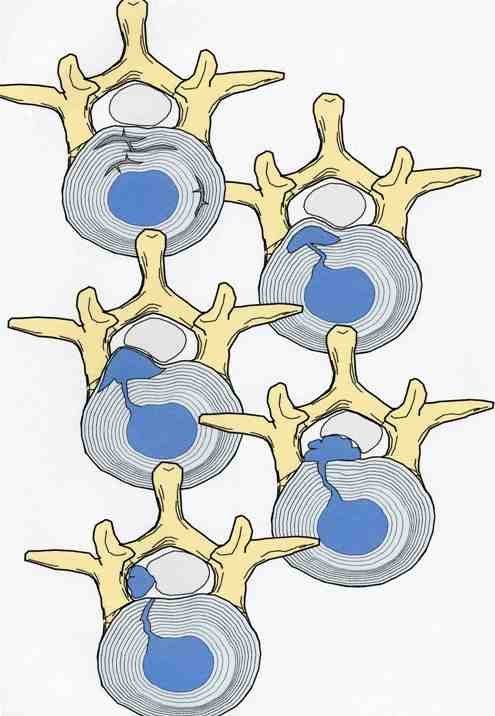
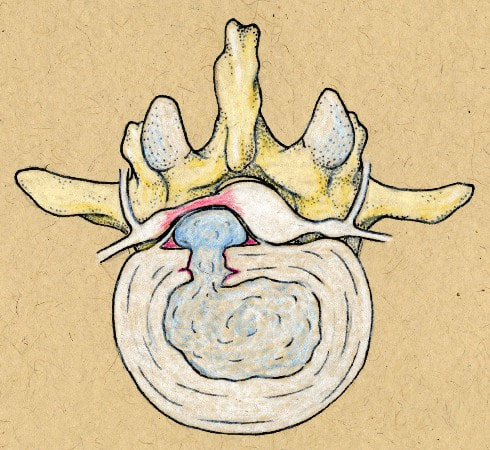
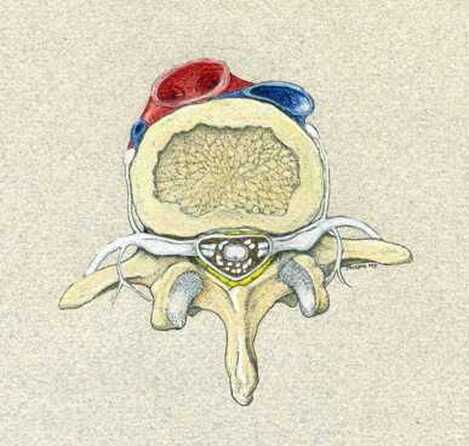
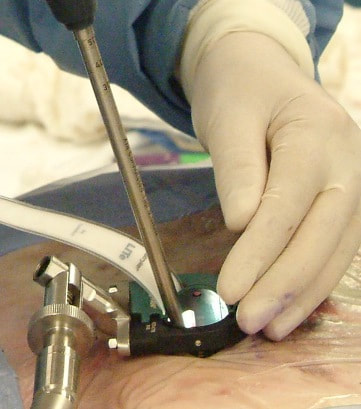
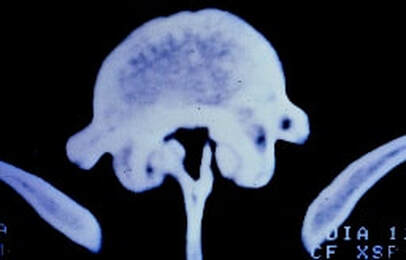
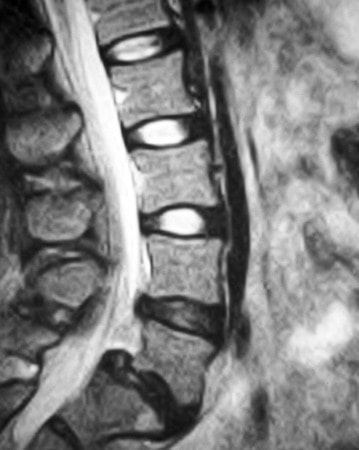
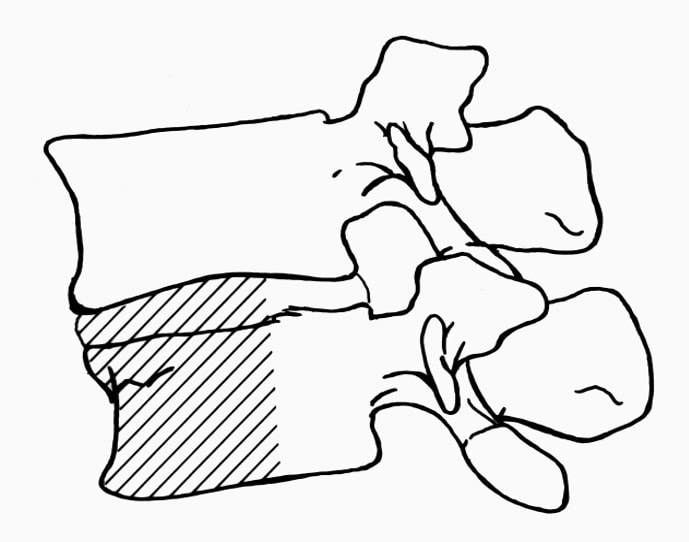
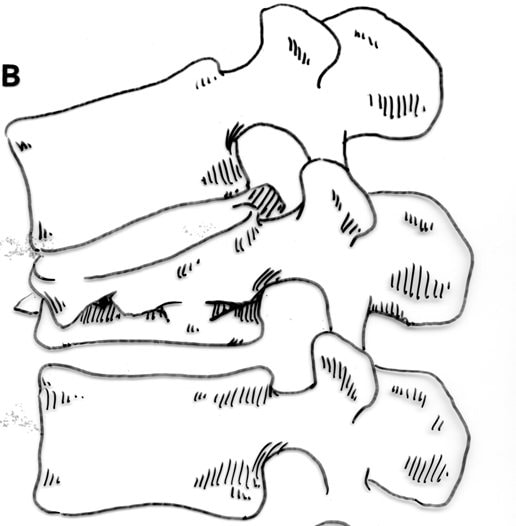
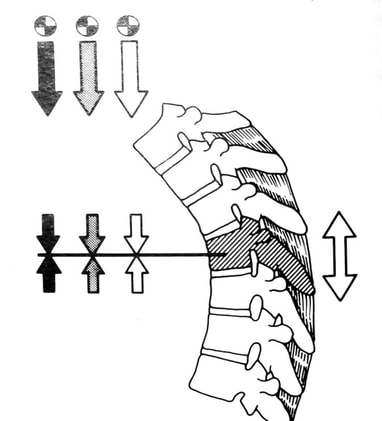
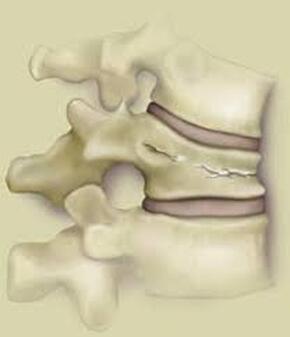
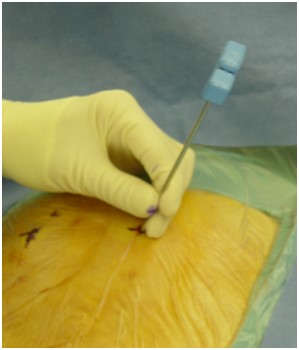
Disc replacement surgery is growing in popularity, but there is still a lot of misinformation out there, and it’s still hard to figure out which facts are FACTS!Cervical disc replacement - or disc arthroplasty - represents a powerful, well-established tool for treating herniated discs and degenerative disc disease in patients who have persistent pain and impaired function due to neck and arm pain, and who want to avoid a spine fusion if they can. So, what’s the role of Disc Replacement Surgery in 2023? There’s more good news and no bad news… Good news!! Most patients with neck pain can recover without surgery: 80-90% will get better, and get back to normal activity with physical therapy, anti-inflammatory meds, rest, activity modifications, chiropractic manipulation…or, in some cases with nothing but time and TLC! For the 10-15% of patients with a serious neck problem that just doesn't respond to time and supportive therapy, many will need an operation. Many of these patients will need a discectomy - a removal of the cervical disc through the front of the neck - to relieve the neck pain and spasm, and the persistent arm pain, numbness, and weakness caused when a spinal nerve root is compressed by a degenerated or herniated cervical disc. This is not a minor surgery, and rarely the first choice in a patient's care, but when pain is bad enough that it interferes with daily function, employment, fitness, and/or sleep…surgery starts to make sense. Who needs spine surgery? We consider surgery the first choice for patients who have more serious issues such as fracture, infection, or tumor. These conditions are relatively rare, often emergencies, and not the sort of thing we usually see in patients with persistent and long-standing neck pain problems. More commonly we are considering surgery for patients with wear and tear and degenerative neck pain problems, or those with a disc herniation related to repetitive trauma or a sudden accident. While we think of surgery as the ultimate treatment for neck pain that won't respond to anything else, we know that surgery is the most reliable solution for most causes of arm pain or weakness (radiculopathy) including disc herniation, cervical stenosis, or spinal instability. Not every type of operation works for every type of spine problems, though, and while disc replacement surgery is an excellent treatment for disc herniations and disc degeneration, it is not a treatment for spinal instability or deformity, and not at all useful for treating tumors, infections, or fractures and dislocations of the cervical spine. Cervical fusion remains the very best solution for each of those problems. For those patients who do suffer neck and arm pain due to disc degeneration or herniation, though, disc replacement – or cervical arthroplasty – is an important option. What is disc replacement surgery? Disc replacement surgery and disc arthroplasty surgery are the same thing. Also referred to as an “artificial disc” the implants used in these surgeries are designed to preserve motion in the spine after a discectomy (removal of the disc) and they have been shown to maintain motion and reduce the likelihood of degeneration at adjacent levels of the spine, something that often occurs in the years following a fusion. They are recommended for patients aged 18 – 70 years, but I, and other surgeons, have had excellent success in selected patients over the age of seventy years. Artificial discs are placed in the neck through the front of the spine (an anterior approach) after a damaged disc has been surgically removed to treat neck pain associated with radicular pain – the arm pain caused by a “pinched” nerve. In the neck, this is exactly the same approach we use for most disc surgeries and all anterior cervical fusions. Disc arthroplasty implants are not experimental or untested. The implants we have now have been in development for over 40 years and similar designs have been available for patient care for nearly 2 decades. There are disc replacement implants specifically designed for the cervical spine (neck) and for the lumbar spine (lower back). They are specifically intended for treatment of degenerated or herniated discs in otherwise healthy patients. There are no discs designed for the thoracic spine, and they are not intended to treat fractures, infections, scoliosis, or spondylolisthesis. And, to answer a pretty common question - you can’t undo an old fusion and put in an artificial disc later! Artificial disc replacement can be carried out as an outpatient surgery, and utilizes many minimally invasive techniques, but it is not “minor surgery”. When it comes to the spine, there is no such thing! The importance of surgeon experience and skill is reflected in the careful diagnosis and plan for treatment, and the skillful approach and placement of the implant. Surgeon experience with disc replacement procedures is important to the outcome here. Ask your doctor what their experience level is and whether they've treated cases like yours before. Disc replacements last a long time. How long? We don’t really know, because – unlike artificial hips and knees – we haven’t seen any of the ones we use today wear out. We have had the opportunity to observe patients from Europe who have had disc implants in place for up to 35 years without failures. As an investigator for early trials of two-level disc replacements, I have followed my own patients for more than 18 years without seeing any cases where the disc has worn out or deteriorated. Who needs disc surgery? Disc degeneration is a process that occurs over time, with wear and tear, age, and physical and environmental stress that causes changes in disc that separates each of the vertebral bodies in our spinal column. Each disc acts as a shock absorber and a slightly flexible joint that allows the spine to move, but only so much. As we age, the molecular components of the disc change, resulting in a loss of water content. The disc loses height, becomes tougher and harder, and becomes a less successful shock-absorber. As this happens, the disc may bulge or protrude into the canal where it can press on the spinal cord or nerve roots, causing arm pain, and it can lose its ability to control neck motion or cushion the small joints during motion, resulting in neck pain As these changes progress we see: Axial neck pain – pain in the joints, muscles, and ligaments of the neck, causing focal pain and stiffness; Referred pain - symptoms over the shoulder girdle muscles that support the neck - the trapezius, rhomboids, and paraspinous muscles and Radicular pain - pain running down the arm and into the hand and fingers in a pattern or distribution typical of a specific nerve level, caused by pressure on the spinal nerve at that level. Radicular arm pain can be uniquely intense and is the symptom that drives most patients to ask for surgery. When these symptoms fail to improve after a trial of non-operative care, that’s when we consider surgery. We generally consider surgery for patients with:
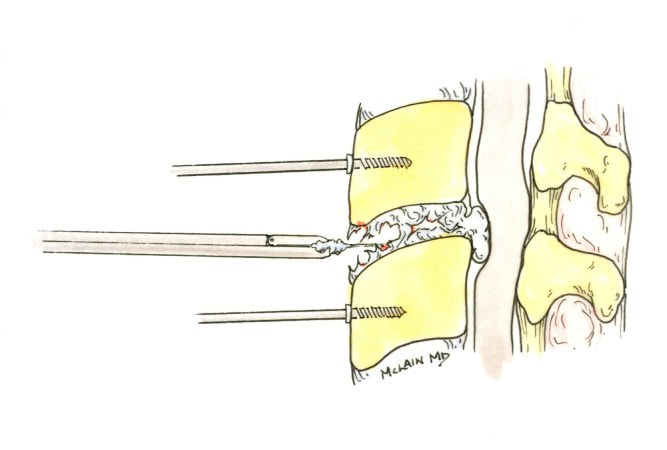
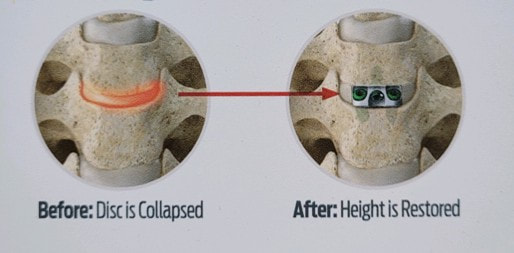
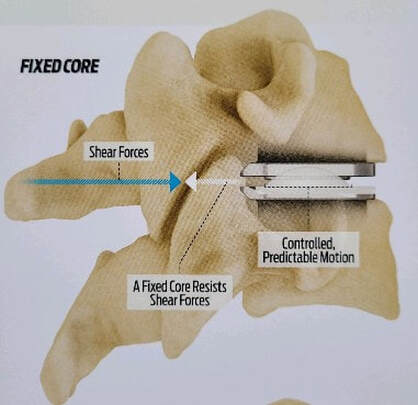
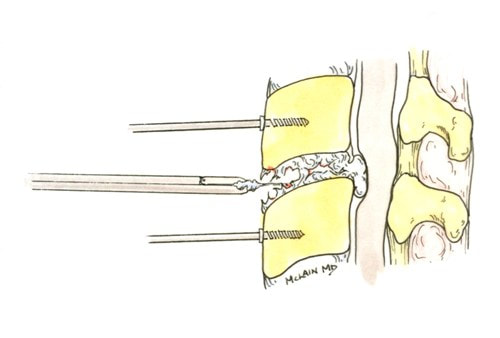
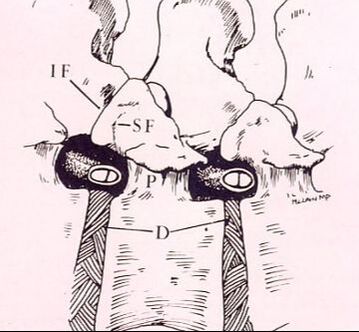
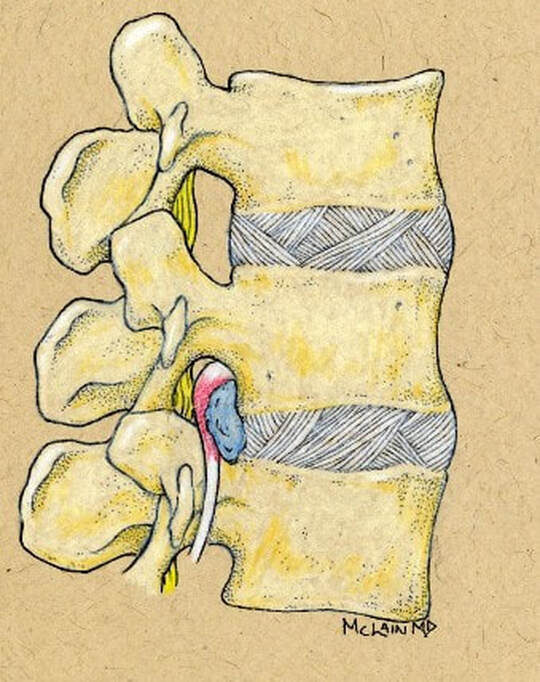
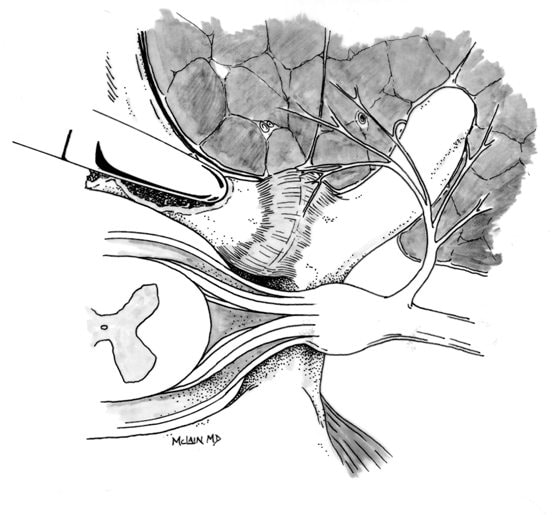
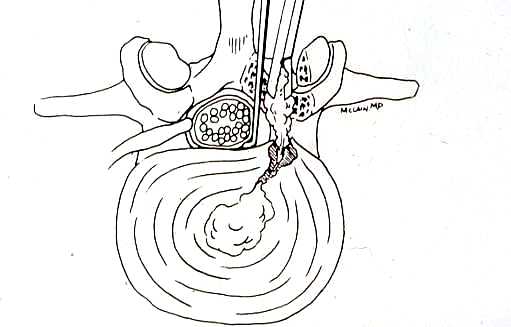
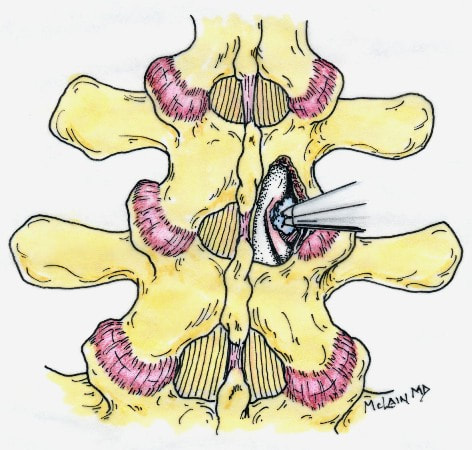
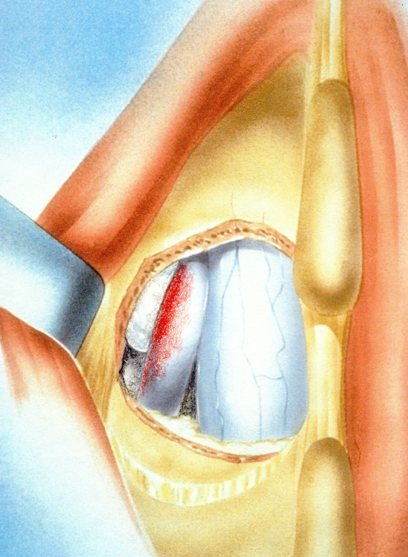
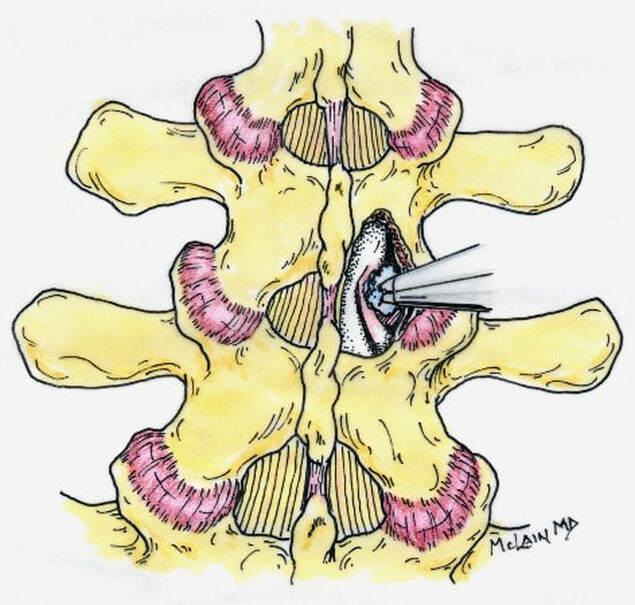
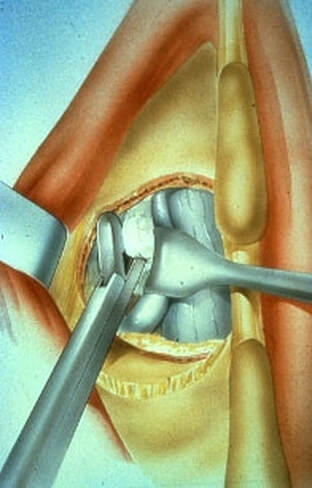
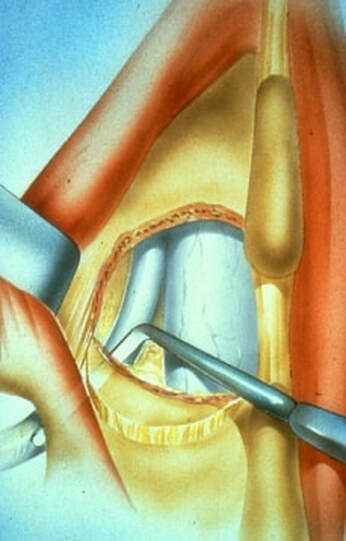
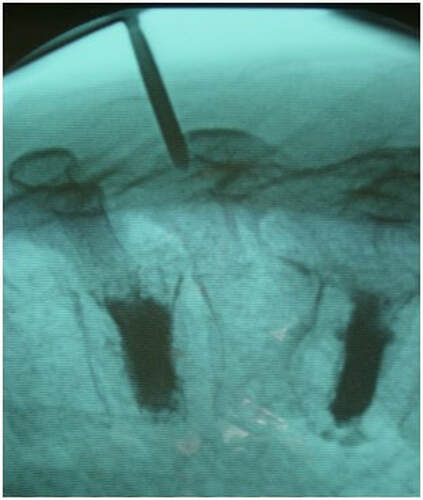
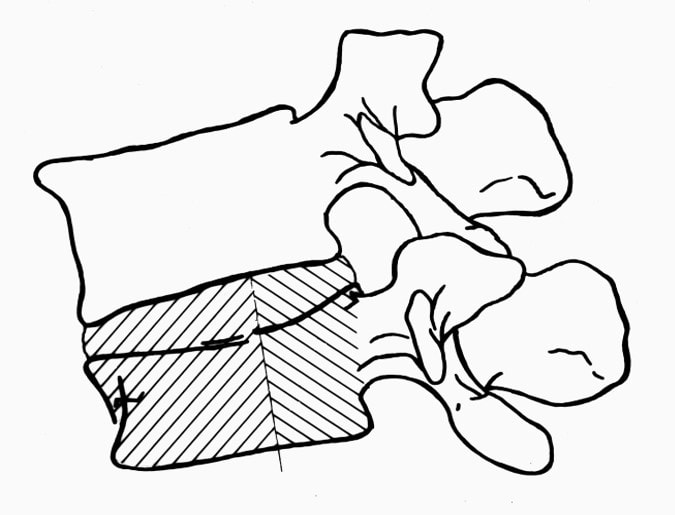
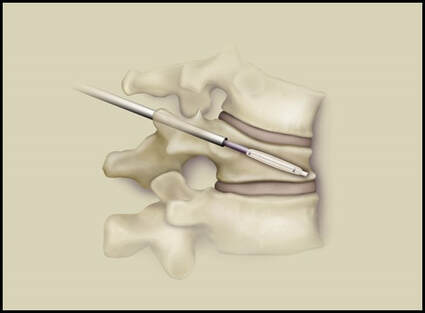
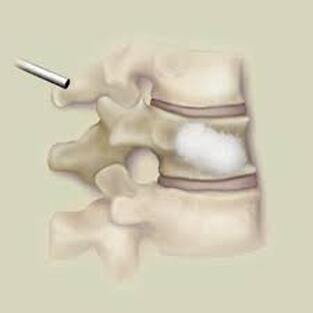
The traditional treatment for cervical disc herniation has been fusion, typically described as an "anterior cervical discectomy and fusion" (ACDF). That’s a surgery through the front of the neck, with complete removal of the disc back to the spinal canal and removal of disc or bone spurs that may be pressing on the nerves. But, why fuse the spine after we get the disc out? The interbody fusion is performed by placing a cage or bone spacer between the endplates of the adjacent vertebrae to restore the intervertebral and foraminal height, immobilize the painful segment, and provide permanent stability. Fusion does all of these things reliably and well! But fusion eliminates motion at the treated level and increases stresses in the adjacent levels above or below, and that can lead to breakdown at that adjacent level, (adjacent level degeneration) sometimes just a year or two after the initial surgery. What does the Artificial Disc do that’s different? The cervical disc arthroplasty or disc replacement is intended for the patient who: - needs the discectomy and would otherwise need a fusion, but - still has motion at the injured level and wants to avoid the down-time required for a cervical fusion to heal, - wants to avoid the risk of non-union (fusion failure) that might require another surgery, and - wants to avoid the risk of adjacent level disease down the road. The approach for the disc arthroplasty, and the removal of the damaged or herniated disc during disc replacement surgery is exactly the same as in the ACDF, but instead of placing the bone or a fusion cage in the empty disc space, disc replacement surgery fills the space with an artificial device that restores disc height and alignment and preserves the motion of the original disc. This allows the treated spinal level to move more naturally, reducing the risk of adjacent level degeneration down the road. And there is no need for prolonged immobilization or restricted activity, as we don't need to "wait for fusion". Who is the best candidate for a disc replacement surgery?
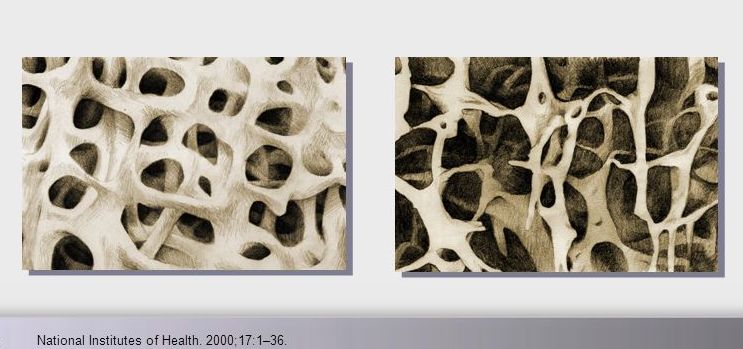
Where will disc arthroplasty work well? Success has been unequivocally demonstrated in the well-maintained but painful disc, in the young and active patients. There are over 150 peer-reviewed publications analyzing investigational FDA trials, long-term follow-up studies, and large multicenter studies to ensure the safety and effectiveness of these implants. These studies have shown that, when used for the correct indications in the properly selected patients, disc arthroplasty provides significant advantages over traditional fusion procedures. They are not "experimental or investigational", and their effectiveness is proven. Do they work in everyone? As we noted at the top of the page, these implants are not intended to treat problems like infections, tumors, or fractures, and they can't undo what has already been done. But they can be considered in almost every patient who would be a candidate for a one or two-level ACDF, so long as the patient has good bone quality and still has motion left at the level to be treated Severe osteoporosis makes any sort of stabilization difficult, and disc replacement is as likely to fail as a simple fusion, but would require a more complex revision that a failing fusion might. And, a patient with no remaining motion at an arthritic level has already started to fuse naturally, and is unlikely to get good motion back with any operation. The disc arthroplasty is a motion-preserving procedure, but it can't undo a solid fusion. What about age? If patients are reasonably fit and bone quality is good, age isn’t a big problem! Large studies and FDA trials of disc replacement have included patients up to age 69, and my experience with patients older than this suggests disc replacements are actually better tolerated than the traditional fusion. At age eighty, some of my fit patients do very well with outpatient disc replacement surgery, returning home within a few hours of their operation, with a soft collar, and no restrictions of daily activity. There has to be good bone quality and good residual disc motion, however. What about activity level? Patients who are athletic or hard working can depend on disc replacements to hold up to their physical demands – the discs are not fragile and the patients don't need to feel fragile either. Patients don't have to restrict their fitness or work activities beyond what makes sense for normal people. What about smokers? Well , first off – stop ! It’s not good for you. However, smoking does not affect the fixation of the disc replacement implant the way it can impede bone formation needed for fusion. Studies to date have not shown smokers to have any poorer outcome after disc replacement surgery than nonsmokers. That's just not the case with fusion, so disc replacement is probably a better choice for you too. With all that in mind, cervical disc arthroplasty continues to offer an attractive and valuable option for most patients otherwise indicated for cervical fusion to treat their neck and arm pain. If you’ve been offered a fusion surgery, ask your surgeon if you’re a candidate for disc replacement! As always, I hope you find this discussion interesting and useful. If you have other questions that I can answer for you, please comment below. If you want more updates on blog posts please like and follow me on my Facebook page.
And feel free to like and share this content with others that might find it beneficial! Thanks for reading. 2/19/2023 Disc Replacement is an Excellent Solution for Adjacent Level Disc Disease: Five Things to KnowRead NowOne of the most concerned groups of patients I see are those who've had a previous cervical fusion - sometimes quite recently -who have now developed new neck pain or a new disc herniation at the level above or level below their fusion. This is called Adjacent Segment or Adjacent Level Degeneration, and it is a well known and common complication of cervical fusion surgery. And, until recently, it has almost always been treated with another fusion. That treatment strategy was the only one available up until ten or fifteen years ago, and it would, as you might guess, tended to start a vicious cycle of fusion and adjacent level herniation that often lead to multiple surgeries and multilevel fusions in many other wise fit and active patients. Even today there are many spine surgeons who will advise their patients in this situation that there is nothing for it, they're going to need another fusion. I've treated enough patients over the years to know that an active, young patient with a 4-level fusion is not often happy with their result. Neck pain is constant, stiffness and limitations in motion are inevitable, and there is always the likelihood that any level that's still mobile is going to degenerate, become painful and require another round of surgery. Again, up until ten or fifteen years ago there really wasn't much else that could be done. That vicious cycle was one reason surgeons and non-surgeons alike would advise their patients to avoid surgery until they just couldn't take it anymore. That approach to neck pain and disc disease is changing, largely due to the advent of disc replacement surgery as an alternative to fusion. Disc replacement surgery is growing in popularity, both because of the interest of patients, but also because of the growing number of surgeons who have been trained in these surgical techniques and who have become familiar with the vast experience of other surgeons who have preformed large clinical trials and extensive peer-reviewed studies to document the advantages and safety of the devices we now have available to us. However, there is still a lot of misinformation out there, and it’s sometimes hard to figure out what facts are important to your individual condition! And that's particularly true when it comes to patients who have an adjacent level disc herniation or degeneration adjacent to a previous fusion. Here are five points that are particularly important for these patients and their care-givers to know: 1. Disc replacement surgery (also called disc arthroplasty) has been available for roughly two decades now, and has an extensive background of supportive research and surgical experience. Use of an “artificial disc” to preserve motion in the spine after a discectomy (removal of the disc) has been shown to maintain motion and reduce the likelihood of degeneration at adjacent levels of the spine, which often occurs in the years following a fusion surgery. Disc replacements have been widely studied in a number of controlled, FDA approved trials, and have proven safety and effectiveness in all of those studies. For those studies, the patients included were very specifically selected, however. Disc replacements were recommended for patients aged 18 – 70 years, typically, but were not allowed for any older patients, patients with other illnesses, and - importantly - patient who had had a previous cervical fusion. It wasn't that they were not expected to work for those patients. Instead, it was known that including patients with too many variables in their background would make the analysis of all of data much more difficult, and could confuse the study. Comparing patients who had had a previous neck surgery to patients who had had no previous surgery would have made these early studies impossibly complicated and could have made it impossible to reasonably document their safety and efficacy for any patient. 2. Artificial discs are placed in the neck using exactly the same surgical technique used for anterior discectomy and fusion surgery, the commonly recommended treatment for adjacent level disease. The surgical approach is through the front of the neck (an anterior approach), and the damaged disc above or below the previous fusion is surgically removed to treat neck pain and the associated radicular pain – the arm pain caused by a “pinched” nerve - in exactly the same way whether a fusion is planned or a disc replacement performed. In the neck, this is the same approach we use for most disc surgeries, but it has to be carried out with added care when a previous surgery has created scarring in the vicinity. That said, there is no greater difficulty with this approach when an arthroplasty is planned than for fusion. In fact, revision surgery for fusion often requires removal of the old plate and screws before the next level can be fused, while this is not usually necessary for an arthroplasty operation. 3. Disc arthroplasty implants have been in development for over 40 years and have been available for patient care for nearly 2 decades. The implants now most widely used have been developed for placement with the most simple techniques and don't require complex surgical techniques such as placing fixation screws or fins, or cutting slots into the bone. In fact, disc replacement is generally focused on the goal of minimal bone removal and minimal soft tissue exposure, which often allows a disc to be placed successfully without ever exposing the fused level above or below. These are implants specifically designed for the cervical spine (neck) and they have very specific applications – treatment of degenerated or herniated discs in otherwise healthy patients. There are no discs designed for the thoracic spine, and they are not intended to treat fractures, infections, scoliosis, or spondylolisthesis. And you can’t undo an old fusion and put in an artificial disc later! But these discs treat the adjacent level cervical discs just as well as they do the primary disc herniations included in those original studies. 4. Artificial disc replacement can be carried out as an outpatient surgery, and utilizes many minimally invasive techniques. So, even in cases where previous surgery has created a scar or affected other levels, disc arthroplasty can still be carried out without the extensive surgery needed to remove and replace a fusion plate with a longer plate, for instance, or move the delicate tissues away from the old fusion bed to get previous hardware out of the way! The importance of surgeon experience and skill is reflected in the ability to recognize the ability to preserve motion at the adjacent level and carry out the motion preserving surgery with the minimum of soft tissue dissection and injury. Your surgeon will provide a careful diagnosis and plan for treatment, and provide the skillful approach and placement of the arthroplasty implant that allows a rapid recovery from surgery and rapid return to function. Surgeon experience with disc replacement procedures is important to the outcome in these revision operations. And, it's ok to ask your surgeon what his or her own experience has been like. 5. Disc replacements last a long time and protect those adjacent levels for a long time as well. With most contemporary arthroplasty implants we use we don’t really know how long they will last, because – unlike artificial hips and knees – we haven’t seen any of the ones we use today wear out. Most patients know either from their own experience or from what they've seen grandparents or family members go through, that hip and knee replacements tend to wear out after 10 - 15 years, and often need to be revised. With disc replacements, we have had the opportunity to observe patients in Europe who have had disc implants in place for 35 years, and we still have not seen any failures. Some of the early designs did not do as well, but those aren't in use any more and have not been for years. In my own experience I have not seen disc replacement fail or require revision. And I have followed my own patients for more than 18 years without seeing any cases where the disc I implanted has worn out or deteriorated. Is this opinion or is this fact? It is important to know that there have been over 150 peer-reviewed publications documenting the results of long-term trials and studies of total disc replacements, both here in the US and abroad. Including investigational FDA trials, long-term follow-up studies, and large multicenter studies to ensure the safety and effectiveness of these implants, almost all of these papers speak to results for primary patients and not those treated for adjacent level disc disease. These studies have shown that, when used for the correct indications in the right patients, disc arthroplasty can provide significant advantages over traditional fusion procedures. Cervical Disc arthroplasty is not experimental or investigational, and the effectiveness of disc replacement is proven. So, is there evidence that the same results can be expected for patients needing treatment for adjacent level degeneration? Is there good evidence that disc replacement can be carried out in a revision surgery as safely and effectively as it can for a primary procedure, or - more to the point - as safely and effectively as for a patient receiving fusion for that revision procedure? There is that evidence, as well as numerous series and smaller reports establishing the suitability of motion preservation for these patients who've already lost a considerable amount of their normal motion due to their first fusion. As an academic surgeon, one of my responsibilities over the years has been to track and document the results of my own patients, to identify problems before others encounter them and to establish the benefits and success of other techniques that other surgeons might subsequently take advantage of. This has also included biomechanical and anatomical studies of surgical technique and implant design, but follow-up of individual patients has always been crucial to good surgical care and the improvement of every kind of treatment. In my most recent analysis of outcomes in patients treated both for primary disc disease and those with disc herniation or degeneration following an older fusion, we were able establish strong support for the clinical opinions discussed above: Comparing adult patients receiving one or two level cervical disc replacements for radiculopathy and/or axial neck pain who had no previous surgery to patients treated the same way, who had adjacent level spondylosis or cervical fusion, and comparing all of them to a series of similar patients treated with fusion for similar degrees of neck pain and radiculopathy we found that: Patients undergoing a primary cervical disc replacement reported excellent satisfaction and pain relief 2 years down the road - 76% percent reported minimal neck pain even with activity, and 36% reported no neck pain at all. 86% reported little or no arm pain at that point, of which 59% reported no arm pain symptoms at all. Compared to this, the patients who had disc replacement for adjacent level degeneration did as well or better - 88% percent reported minimal neck pain with activity, of whom 50% reported no neck pain at all, and 100% reported little or no arm pain at 2 years, of which 75% reported no arm pain symptoms at all! Compared to patients having cervical fusion - well, they did well also, but as early as 3-4 years after surgery 18% were reporting moderate to severe neck pain, and a few were experiencing moderate arm pain. I was pleased to present the preliminary report of this peer-reviewed material at the MidAmerican and the Western Orthopaedic Association Annual Meetings in 2022. While these numbers are too small to prove anything, they certainly support the use of a disc replacement device in patients who've already lost some neck motion, as opposed to forcing them to undergo additional fusions. And what about the safety? In our analysis of these patients - none of the patients in any group suffered a complication either during or after surgery, and none of the patients treated for adjacent level degeneration has required any other surgery. Any neck operation requires superior care and technique to get a good result without complications. None of these procedures should be considered minor surgery, even when they can be performed as outpatient operations.
So, if you’ve been told you need to have a neck fusion, for a primary disc herniation or disc degeneration or for a problem that has arisen following a previous fusion, it’s ok to ask “is there another way - a better way - to treat this?”. It's worth getting a second opinion to see if disc arthroplasty might be that better way for you! I hope you found this informative and interesting! You can learn more about disc replacement surgery, and other types of spine surgery and treatment, by checking out more sections of this website, and you can follow me on Linkedin or Facebook to learn about new updates and post that may help you take care of your back and neck. Thanks for reading! Paleopathology: Musculoskeletal Disease in Early Man |
Details
AuthorI'm Dr. Rob McLain. I've been taking care of back and neck pain patients for more than 30 years. I'm a spine surgeon. But one of my most important jobs is... Archives
January 2024
Categories |















































 RSS Feed
RSS Feed