What can you do to care for you back and neck when you're out in the garden?My patients love to garden, and no matter what - back pain, neck pain - nothing's going to keep them out of the garden for long. But there are things you can do to keep your back and neck in good shape while you do that hard work you love so much! Thanks for watching!
Let me know in the comments if there are questions you'd like me to answer about your back or neck problems, or about spine surgery in general. And feel free to share this with others.
0 Comments
While insurance companies continue to explain that their “process” is simply a means of protecting patients from unnecessary or unproven procedures,it is clear that the process is becoming so widespread that anyone can end up facing a denial for treatment – delaying care and requiring a formal “appeal” for almost any form of medical care. Different insurers handle the process different ways, but all use it. Doctors continue to incorporate algorithms into their notes and documentation to cover every possible question your insurer could ask, but, then, the insurer can always ask something else that has never come up before, or more commonly request written documentation from a third party to support the patient’s own report, in essence saying “Prove it!”. And this denial of coverage often comes within 24 hours of the scheduled surgical date, making a response difficult, impossible, or fruitless. The usual outcome is that your doctor will have to have a “peer-to-peer” conversation (argument) with another doctor (often retired, employed by the insurer), to convince them that the surgery is necessary and appropriate. Usually this is successful, but it helps (is absolutely necessary) if your doctor has ALL THE AMMUNITION he/she needs to win that argument. Patients often assume that, for one reason or another, this won’t affect them. Here are 5 (OK, 7) ASSUMPTIONS patients commonly make before getting DENIED by their insurance company:
5. My health is at stake – surely they don’t want me to get sicker? Remember this – your insurer didn’t say you couldn’t have surgery, they said they wouldn’t pay for it. The AMA suggests that one of the proposed benefits of pre-approval denials – the prevention of unnecessary treatment and costs – often borne by employers, has not been seen, and that an additional cost of prolonged and sometimes permanent disability for their workers has now been documented, and attributed to either delay treatment, or patients’ frustration and decision to abandon effective treatment because of denials. To that point the AMA survey found that:
6. Well, as long as I get the surgery done, they’ll have to pay afterwards. That’s not a reliable assumption even if you get the pre-approval in the first place. Post-treatment denials are not uncommon and require a another round of appeals if your hospital is going to recoup the expenses of the hospitalization and surgery without turning to you. The denial letter will again refer to “your healthcare providers” either lack of documentation or a mistake in billing, but that mistake can consist of absolutely perfect paperwork being read incorrectly by the insurer – for instance a reviewer not recognizing the difference between arthrodesis (fusion) and arthroplasty (joint replacement). 7. Well, if my doctor does a good job with the peer-to-peer review this should get settled pretty quickly, right? Unfortunately, not so. Roughly a third of the peer-to-peer reviews I engage in start with “So what did you call us for?” When I respond that I was offered a chance to appeal their denial decision I am informed that, no – I was offered a chance to call and discuss it, but that the denial was made based on “a Board decision”. I was informed that the company had decided at the corporate level not to cover that type of treatment and that there was no opportunity to discuss, appeal, or debate the denial. “Thanks for calling”. Or as one neurosurgeon/reviewer told me – “your right, there’s no reason to get an MRI for this patient’s compression fracture, but that’s our corporate policy. She (the patient) must have an MRI and then resubmit the request”. They then refused to approve the MRI! So, here’s my advice:
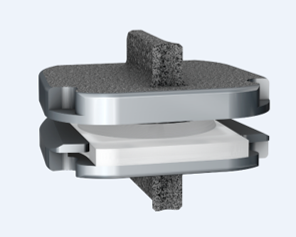
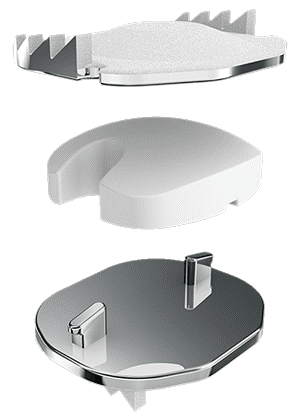
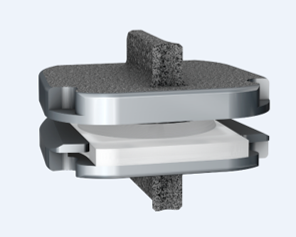
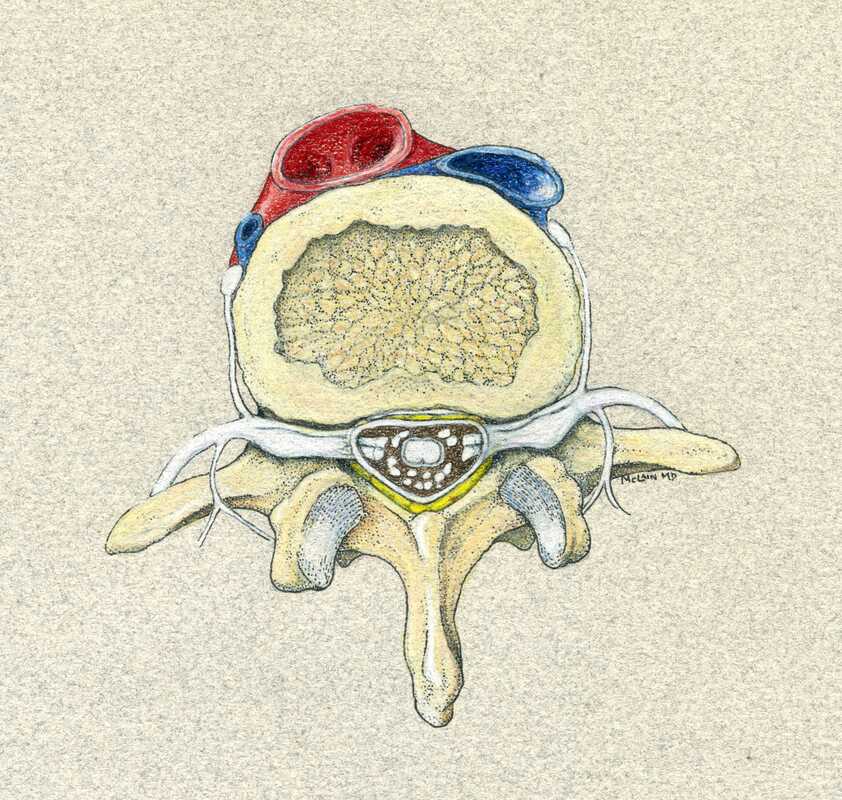
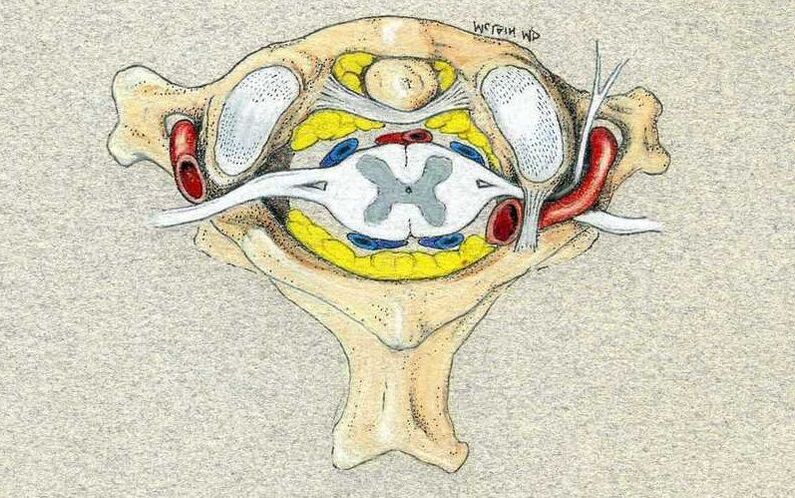
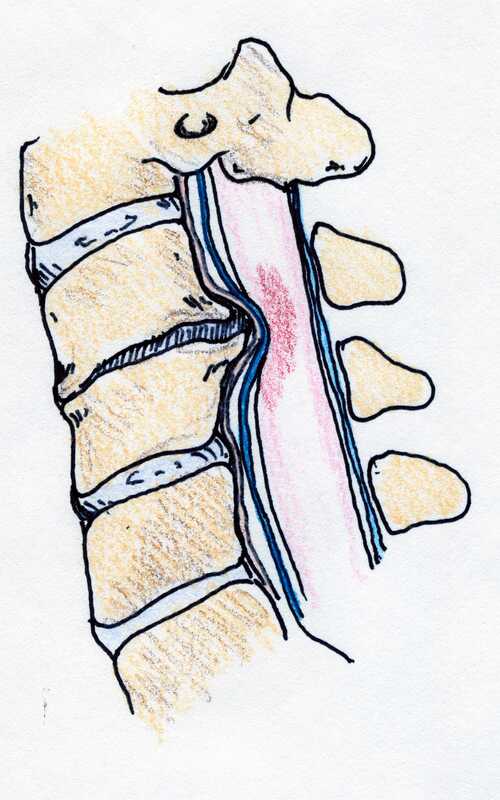
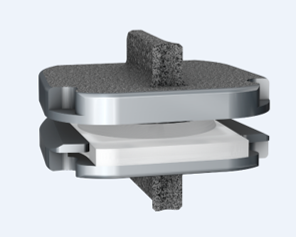
Get your records, keep your records, and copy your records like you were preparing for a tax audit. Know who provided your care, when and where. Bring copies of your physical therapist or chiropractors treatment notes with you. Don’t fudge the dates – if you tell me “sure – I’ve had a full course of physical therapy” I’ll believe you, but if it turns out it was three visits two years ago, there’s a real likelihood your surgery will get delayed or flat-out denied. Don’t cut corners – if your doctor prescribes physical therapy but you just don’t want to go, there’s not much anyone can do if your insurer flags your chart. If you do go, and it’s just too painful – GET YOUR THERAPIST TO DOCUMENT THAT CLEARLY – and provide that documentation when you come to see your surgeon. Bring your imaging studies – x-rays and MRI – on a CD so your doctor can read them and plan the best treatment for you, BUT ALSO – bring the Radiologist’s printed reports for those studies so they can be submitted with your treatment application. This was intended as a brief note, but so many of my patients are being impacted by this process now that it is crucial that you be prepared and understand the process a bit. It won’t help to get frustrated with your doctor’s clinic staff or schedulers. They often fax 20 – 30 – 40 pages of material to your insurer, 2 or 3 times to make sure everything is in order...only to get a one page fax the day before surgery, without explanation, stating that the surgery is denied for “lack of documentation”. And, if you end up embroiled in this process, this is one time that writing your senator and congressman wouldn’t be a bad idea, as these issues are being reviewed in congress. Your story could be important to changing this system! Thanks for reading, and let me know what other questions you might have! By now you’ve heard a lot about artificial discs, or disc arthroplasty, as a treatment for certain kinds of neck problems including cervical disc herniation or cervical disc degeneration.If you’re looking for scientific papers on the subject, you can find over 150 peer-reviewed publications on Pub-Med or in the Scientific and Medical Journals that focus on surgical treatment. But what if you just want to know what they look like and how they work? Well, let’s break it down! What is an artificial disc? An artificial disc is used to replace the damaged intervertebral disc that is removed during discectomy as treatment for a disc herniation or disc degeneration. Placement of the artificial disc, more commonly referred to as a disc arthroplasty or cervical disc replacement, fills the gap left when the original disc is taken out. In so doing the artificial disc restores the original, normal disc height, holds the adjoining vertebra in normal alignment, and preserves a small amount of motion in flexion and extension, side to side rotation, and left and right side-bending – about the amount the normal disc had when it was healthy. A spinal fusion – the traditional solution after discectomy – can do those first two things very well, but it eliminates all motion at that level, leaving the rest of the spine to take up the slack. How does the disc replacement work? The disc replacement device, or implant, is designed to insert into the disc space – the gap left after the disc has been taken out – with minimal removal of normal bone or ligament tissues, and is held in place with small teeth that grab the bone, and with the normal tension of the remaining soft tissues holding it firm. The bone of the vertebrae will eventually grow directly into the top and bottom plates of the device making the fixation permanent, but right from the start the fit of the specific disc designs is such that loosening or slippage of the device is very rare, even with early motion and activity. So, they don’t need to be screwed in or cemented into place, and you don’t need to wear a hard collar or immobilizer while recovering from surgery. How are disc replacement implants designed? There have been many different designs of artificial discs created over the last 40 years, and a lot of different materials have been tried from one time or another. Spine surgeons have benefited A LOT from the much longer and sometimes fraught experience of our total joint colleagues who have been studying these issues for many decades longer. The implant designs that I use now are all FDA approved, studied in numerous scientific trials, and have been in use around the world for at least a decade in each case, and much longer in some cases. The primary design for each of the implants I use is the same: Each disc design has three parts: two metal plates – one top and one bottom - and a plastic insert or spacer in the middle. The plates are made of a mix of metals commonly used in spine and joint replacement surgery (cobalt, chromium, and molybdenum in some cases, and titanium in others). The plates typically have either teeth on the top and bottom that help hold the plates to the vertebrae, or small thin “keels” that slot into the bone above and below. The teeth or keels are pressed into the bone without any bone removal, which makes the implant designs I use easy to place properly, without cutting away normal bone. The surfaces of the top and bottom metal plates are typically sprayed with a coating of a bone forming material (hydroxyapatite) that stimulates the vertebral bone to grow and attach to the metal plates for long term stability. The plastic insert that fills the space between the plates differs from implant to implant. In most implants the insert is made from a high molecular weight polyethylene, a material with enough density to resist wear and deformation over time, but “slick” enough to provide very little friction as it slides back and forth against the upper and lower plates. This is the same strategy and material used in our most successful and long-lasting hip and knee replacements. The insert is designed to move a little back and forth and side to side as you move your neck, mimicking your natural joint motion. How big is the implant? They come in different sizes, in order to properly fit different size patients. (Interestingly, your body size does not necessarily tell me much about the size of your spinal elements: some very big people have a surprisingly small bone structure, and vice versa!). Typically, though, the implant is not much bigger than the size of your thumbnail, and not taller than two or three quarters stacked together. The four disc replacement implants I current use are all FDA approved and well-studied across the globe. Full disclosure – I have been asked to teach surgical techniques to other surgeons from time to time, and I do participate in Investigational trials for some implants ( I was a Principle Investigator for the original MobiC two-level FDA study 15 years ago, and am an investigator for Centinel Spine’s two-level Investigational Device study now), but I am not a paid consultant for any of these companies. So, I can honestly say I pick the implant that suits my patient’s situation best, each time! MobiC – ZimVie is a new name for a long-established company, and the most widely used two-level implant in the US. You can learn more about their implants here. Pro-Disc-C – One of the first to bring an artificial disc to the lumbar spine world, they have a long-established and successful product for single level surgery, and Centinel Spine is sponsoring an ongoing investigational study for their new implants for two-level surgery. M6 – Provided by Orthofix, this implant has a unique central core that also provides a little more cushion, in theory, than the solid high molecular weight polyethylene cores, and fits certain disc configurations very well. Simplify – A newer entry provided by Nuvasive, this implant has titanium plates top and bottom, which eliminates any concern for those with metal allergies, and is approved for two level use.
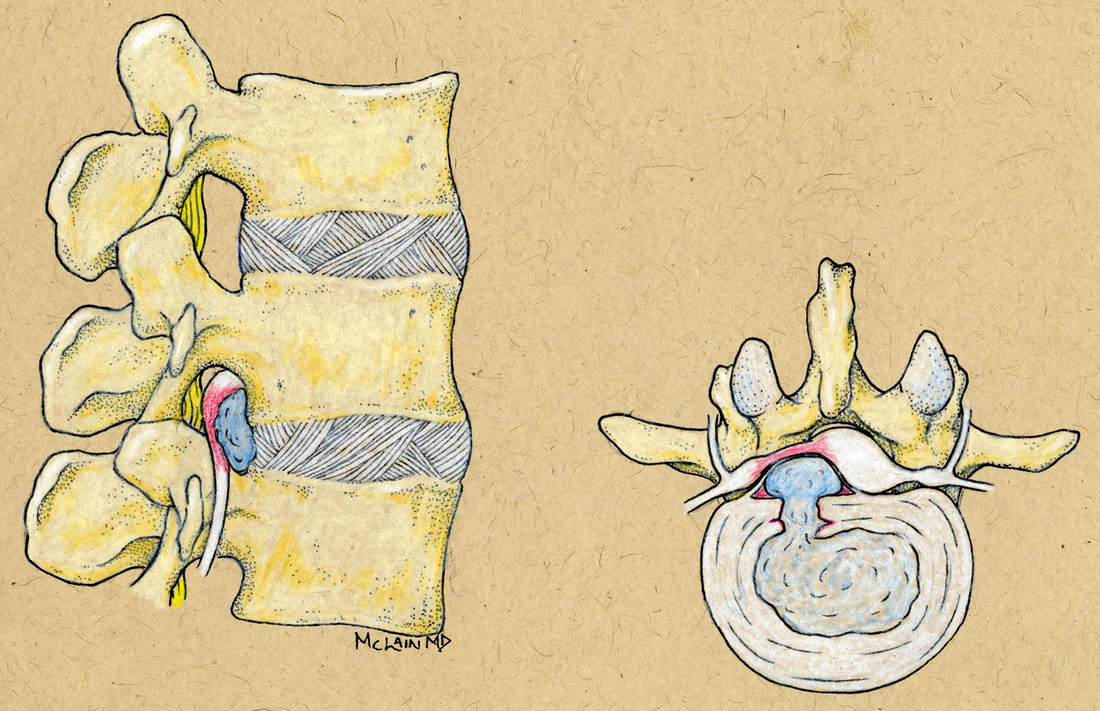
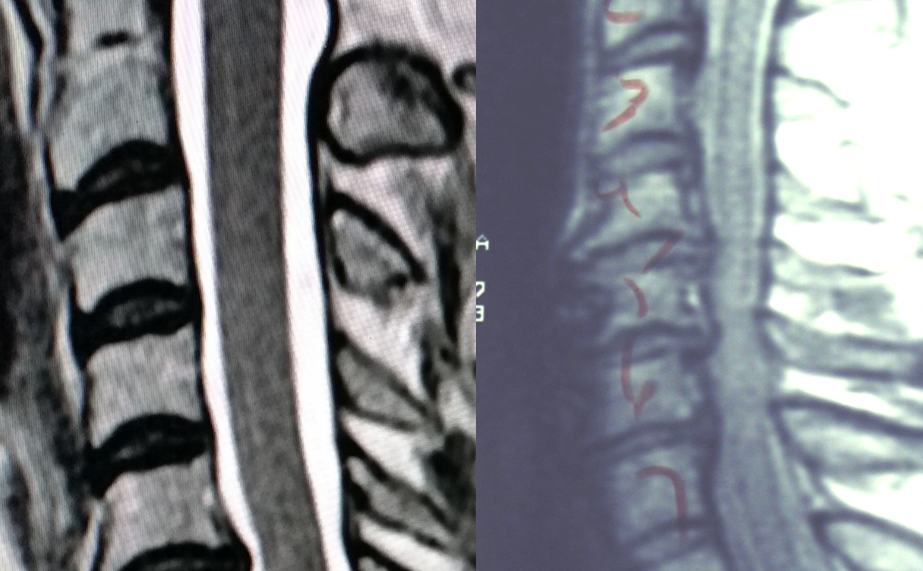
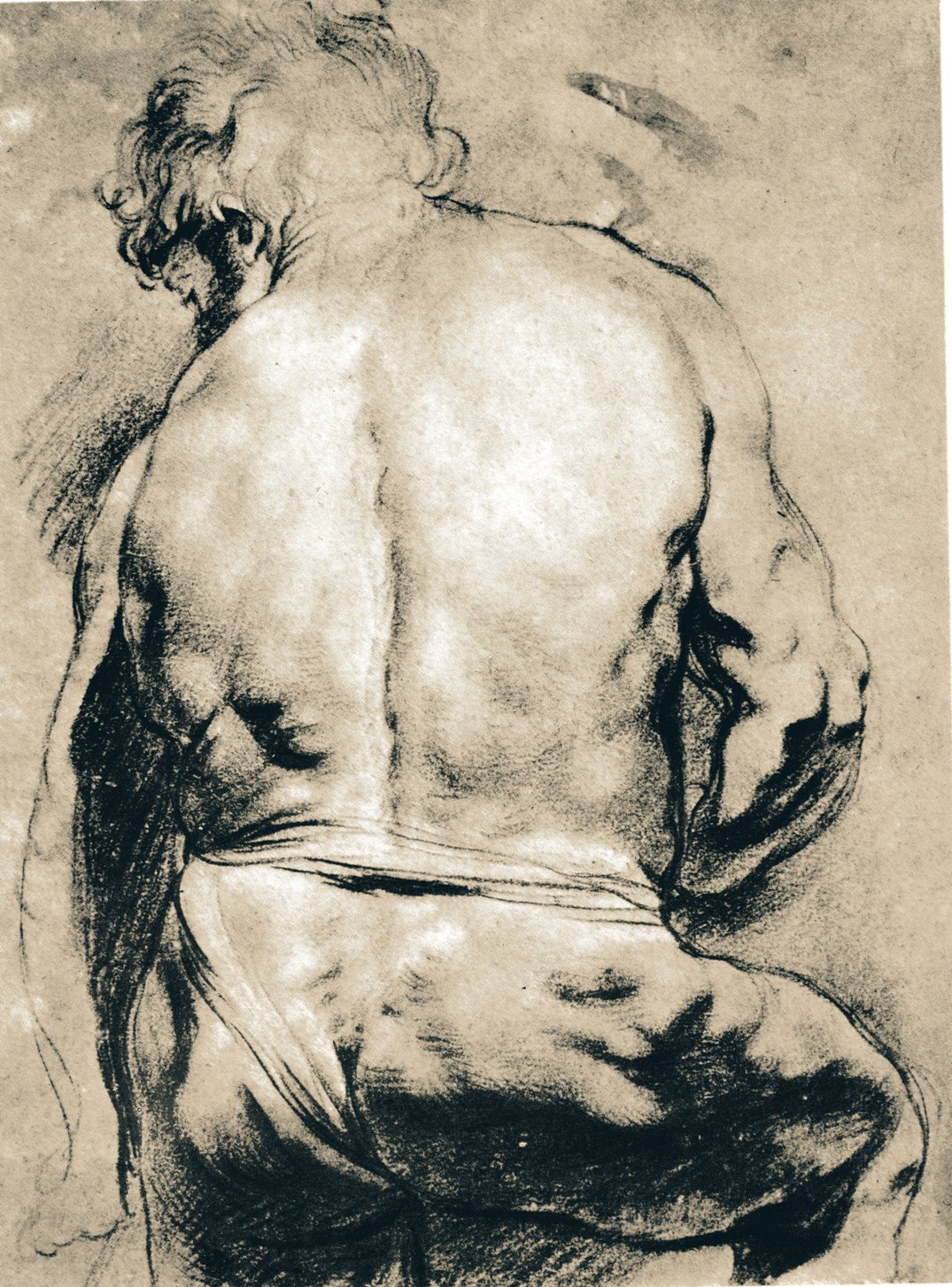
Thanks for reading! I hope you found this both interesting and informative. Feel free to Like and Share this content and please comment to let me know what other questions you might have! Cervical Disc Arthroplasty: Motion preservation for patients with severe neck pain and arm pain due to disc herniation or degenerative disc disease. Disc replacement surgery represents a powerful, well-established tool for treating disc herniations and cervical disc disease in selected patients. That’s good news for patients who have persistent pain and dysfunction due to neck pain, who still want to avoid a spine fusion if they can. So, what’s the role of Disc Replacement Surgery in 2022? There’s good news and bad news… Good news!! Most patients with neck pain recover without surgery: 80-90% will get better, and back to normal activity with physical therapy, anti-inflammatory meds, rest, activity modifications, chiropractic manipulation…or, in some cases with nothing but time and TLC! Bad News!! About 10-15% of patients with a serious neck problem will eventually need surgery. They’ll need an operation to relieve persistent arm pain due to a herniated disc, arm pain and weakness due to nerve root compression caused by disc degeneration, or surgery to treat instability or deformity. When persistent neck and arm pain are annoying, we can treat those well with a number of different non-operative strategies – physical therapy, manipulation, oral medications, or injection therapy. But when pain is bad enough that it interferes with daily function, employment, fitness, sleep…surgery starts to make sense. Who needs spine surgery? We consider surgery for patients who have structural neck pain problems, such as disc degeneration, instability, deformity or more serious issues such as fracture, infection, or tumor. We also depend on surgery as a reliable solution for many causes of arm pain or weakness (radiculopathy) including disc herniation, cervical stenosis, or segmental instability. Not every type of operation works for each of these problems, though, and each has its strengths and its drawbacks. Disc replacement surgery is an excellent treatment for disc herniations and disc degeneration, but it is not a treatment for spinal instability or deformity, and not at all useful for treating tumors, infections, or fractures and dislocations of the cervical spine. Cervical fusion remains the very best solution for each of those problems. For those patients who suffer neck and arm pain due to disc degeneration or herniation, disc replacement – or cervical arthroplasty – is an important option. Who needs disc surgery? Degeneration of the Intervertebral Disc causes changes in disc, which sits between each of the vertebral bodies and acts as a shock absorber and slightly flexible joint. As we age, the molecular components of the disc change, resulting in a loss of water-holding capacity, and a progressive loss of elasticity and compressive strength – the disc becomes a less successful shock-absorber. On x-rays we see: Bone spurs (osteophytes) form around the facet joints and edges of the discs themselves Disc damage that causes bulging and herniation Loss of normal mechanical stability, loss of disc height, and loss of normal neck posture We can even see structural deformity These changes go along with the symptoms we see: Axial neck pain – pain in the muscles and ligaments of the neck, stiffness, shoulder and back pain; Referred pain - symptoms over the trapezius, rhomboids, and shoulder blades Tension myositis - muscular pain, often causing headaches; and Radicular pain - pain in the spinal nerve distribution causing pain down the arm and into the hand and fingers Radicular arm pain is the symptom most commonly requiring surgery. When these symptoms are severe, interfering with fitness health, and normal rest, and when they fail to improve after a good trial of non-operative care, that’s when we consider surgery. The general rules for choosing surgery for a patient start with the symptoms:
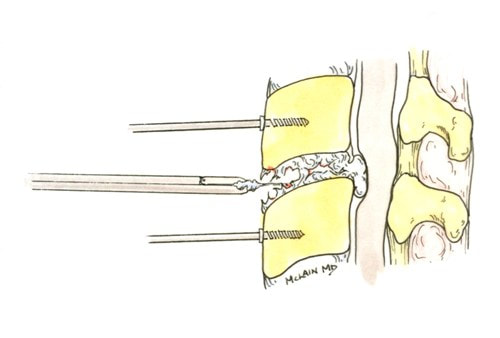
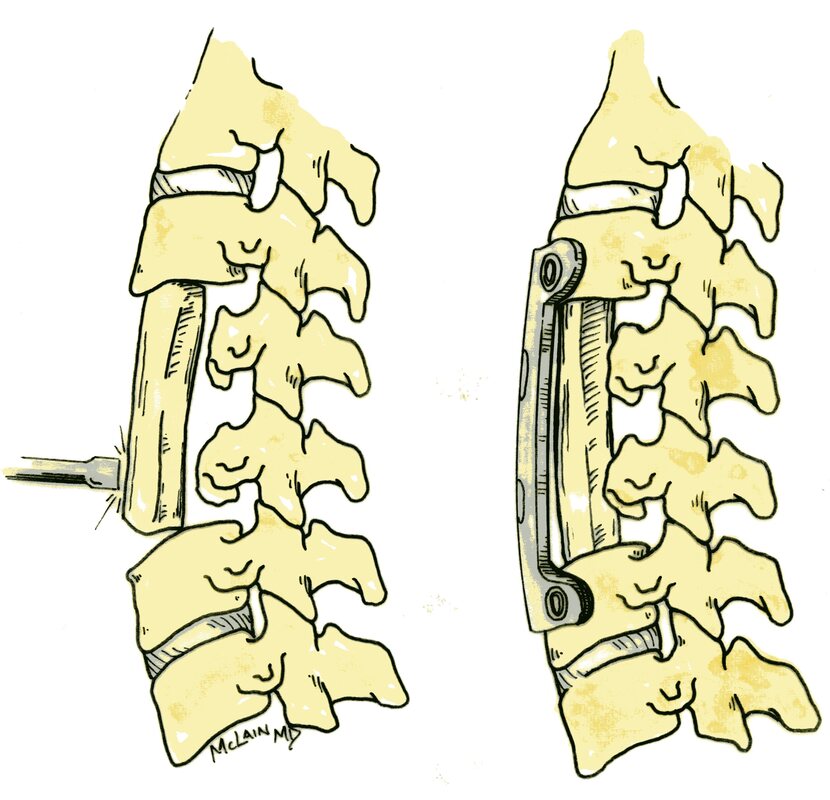
The traditional treatment for cervical disc herniation is an anterior cervical discectomy (surgical removal of the disc) and fusion (ACDF). That’s a surgery through the front of the neck, through which the disc is removed all the way back to the spinal canal. But, why fuse the spine after you get the disc out? The interbody fusion (placing a cage or bone between the endplates of the adjacent vertebrae) restores intervertebral and foraminal height, immobilizes the painful segment, and provides permanent stability. But it eliminates motion at the treated level and increases stresses in the adjacent levels above or below, and that can lead to breakdown at that adjacent level, (adjacent level degeneration) sometimes just a year or two after the initial surgery. What does the Artificial Disc do that’s different? The cervical disc arthroplasty or disc replacement is intended for the patient who would otherwise need a fusion. The approach for the disc arthroplasty, and the removal of the damaged or herniated disc is exactly the same as in the traditional ACDF procedure, but instead of placing bone or a fusion cage in the empty disc space, disc replacement surgery replaces the damaged intervertebral disc with an artificial device that restores disc height and alignment and preserves the motion of the original disc. This allows the treated spinal level to move more naturally, reducing the risk of adjacent level degeneration down the road. Who is a good candidate for a disc replacement?
Where will disc arthroplasty work well?
Success has been unequivocally demonstrated in the well-maintained but painful disc, in the young and active patients. What about older patients? If patients are reasonably fit, and bone quality is good, age isn’t a big factor! Studies of disc replacement have included patients up to age 69, and my experience with patients older than this suggests disc replacements are just as successful, and better tolerated than the traditional fusion. What about activity level? Patients that are athletic or hard working can depend on disc replacements to hold up to high demands – they are not fragile. What about smokers? Well, first off – stop! It’s not good for you. However, smoking does not affect the outcome of disc replacement surgery the way it can a fusion, so disc replacement is probably a better choice for you too. Here's the caveat:
With that in mind, cervical disc arthroplasty offers an attractive and valuable option for most patients otherwise indicated for cervical fusion to treat their neck and arm pain. If you’ve been offered a fusion surgery, ask your surgeon if you’re a candidate for disc replacement! As always, I hope you find this discussion interesting and useful. If you have other questions that I can answer for you, please comment below. And feel free to like and share this content with others that might find it beneficial! Any good medical exam starts with a careful history. That means answering some important questions, so be prepared!Back and neck pain are common problems that most all of us will experience at one time or another. However, the cause of each person’s pain and the way it affects their life and function can differ significantly. One of the most common causes of failed spine surgery and failed back care is failure to make the correct diagnosis up front, and the subsequent failure to provide the best treatment thereafter – doing a surgical procedure that wasn’t helpful or failing to operate when someone really did need it. One of our most important tools in medical diagnosis – of any kind – is called the “History”. Without a good history, we tend to make assumptions, and if they are the wrong assumptions then we can start down the wrong path when it comes to treatment. That can lead to delays in recovery, unnecessary procedures, or a poor outcome all together. No one wants that! So, your doctor will want a full and accurate history to help them understand what your particular problem is and how it affects you, so they can provide you the very best and most specific care. Here are Six Questions you should be able to answer for your Back Doctor when you come to talk about back and neck pain or back and neck surgery: 1. What can I do for you today? “Just fix me” sounds cute, but it’s not a helpful answer. Tell me what brings you in today – “I’ve had back pain for years, but for the last 3 – 6 months I’ve been getting terrible leg pain and it worries me” or “ I’ve been diagnosed with a neck strain, but it’s not getting better and my doctor thinks I need to see a specialist”. It’s OK to say “I’m not interested in surgery, I just want to make sure it’s not something serious!”. 2. Where does it hurt? – Sounds simple enough, but every day I meet patients who said “neck pain” on their intake form yet immediately describe burning pain running down their arm to their hand as their real problem. This is important information and it’s important to be thoughtful and specific in your description. And, if the answer changes with activity or time of day that’s important too. “When I first get up my pain is right in the middle of my back – low down, but after I’ve been up and standing, it starts to run down the back of my legs to my feet and toes. Is that weird?” No – it’s important information. 3. How bad is your pain? This is always a hard question to answer, because we each experience pain in different ways at different times. The best way to measure pain is sometimes in terms of what it prevents us from doing. If the pain is severe enough that it’s interfering with your ability to sleep, exercise, and/or work, that’s important. If non-operative treatments don’t get you significant relief, surgery might be a serious consideration. If it’s keeping you from enjoying more than three or four rounds of golf each week, that’s important too, but it suggests you’re functioning pretty well, and a sports/rehab approach might be right for you! 4. How long have you been having pain? It’s important to be clear – I recently had a long conversation with a patient who reported that her pain had started “about three weeks ago”. After looking through the patient’s records I asked why they had had previous x-rays and MRI studies. “Oh, I’ve had back pain for years. But this time it’s been going on for three weeks”. It’s okay to be a little more detailed – “I’ve had back pain for years, but the leg pain didn’t start until the last six months, and it was just last month that it became severe and the numbness and tingling started”. 5. What have you been doing to treat the pain? Your doctor will want to know, and your insurance provider – Medicare, Medicaid, or any other – will quite literally tick off the boxes on previous treatments before they approve any surgery, injection therapy, or even an MRI. “I take an anti-inflammatory medication regularly, with some benefit. I’ve had a complete course of physical therapy, starting in…and ending in…(know the dates), and it didn’t help me much”, or “I tried to do physical therapy, in …(know the dates), but it made my pain worse and I had to stop”. If you’ve had injections or other treatment, make a note of when that was, where it was, and who your doctor was. “I’ve had injections recently, but they didn’t help or at least not very long. They were done by Dr. …, and they were epidural injections/selective nerve root blocks/trigger point injections/facet blocks…”. If you’ve had a previous operation, who did it and what did they do? Bring records with you when you can. When insurance companies deny treatments or demand an appeal for treatment, it’s usually based on lack of previous treatment or lack of documentation of previous treatment. 6. Are you working at your regular job right now? This isn’t just a question about your insurance, but one about how your pain is disrupting your life. “I am not working at my regular job, which involves a lot of bending, lifting, or twisting, but my company is great and they’ve got me a light duty job that’s easier to do” is a completely different answer and situation from “ my boss hates me and says I can’t come back unless I can go back to the loading dock”.
But it’s just as important to know that, if you work in the home, you can’t carry a load of laundry, pick up your children or do your household tasks. In either case it’s appropriate to ask the question: Do you need a back operation, or do you need a better job or more help in the home? Making a correct diagnosis and putting together a sound treatment plan depends on understanding where your pain is coming from, how it’s affecting your life and impairing your function, and understanding whether it’s likely to respond to a program of non-operative treatments and therapy or whether there is likely to be a need for surgery. So don't get frustrated with all the questions - it's your chance to guide your doctors in the right direction. If you can provide a clear and accurate History for your doctors, its much more likely that you’ll get the care you need, when you need it, with the best possible outcome. Thanks for reading! Feel free to Like and Share this content and let me know what other questions you might have! Five (OK TEN) things no back patient should ever do…how many are you guilty of?
So, please be careful…I want you to be active, but take care of your back and use good common sense!
I hope you find this discussion interesting and useful. If you have other questions that I can answer for you, please comment below. And feel free to like and share this content with others that might find it beneficial! If you’ve been to more than one doctor for a neck pain problem, you may have been bombarded by confusing terminology and a lot of similar sounding words. Do you have radiculopathy or myelopathy? Your chiropractor said you have a somatic disorder, and your physical therapist called it myofascial pain, and somewhere it showed up on a report as cervicalgia. Could this be neuropathy? Myopathy? |
Details
AuthorI'm Dr. Rob McLain. I've been taking care of back and neck pain patients for more than 30 years. I'm a spine surgeon. But one of my most important jobs is... Archives
January 2024
Categories |




















 RSS Feed
RSS Feed