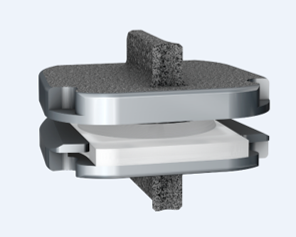
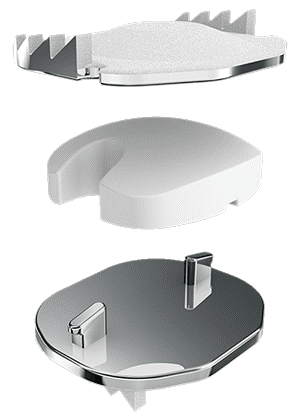
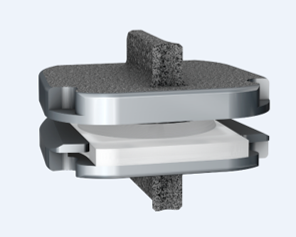
By now you’ve heard a lot about artificial discs, or disc arthroplasty, as a treatment for certain kinds of neck problems including cervical disc herniation or cervical disc degeneration.If you’re looking for scientific papers on the subject, you can find over 150 peer-reviewed publications on Pub-Med or in the Scientific and Medical Journals that focus on surgical treatment. But what if you just want to know what they look like and how they work? Well, let’s break it down! What is an artificial disc? An artificial disc is used to replace the damaged intervertebral disc that is removed during discectomy as treatment for a disc herniation or disc degeneration. Placement of the artificial disc, more commonly referred to as a disc arthroplasty or cervical disc replacement, fills the gap left when the original disc is taken out. In so doing the artificial disc restores the original, normal disc height, holds the adjoining vertebra in normal alignment, and preserves a small amount of motion in flexion and extension, side to side rotation, and left and right side-bending – about the amount the normal disc had when it was healthy. A spinal fusion – the traditional solution after discectomy – can do those first two things very well, but it eliminates all motion at that level, leaving the rest of the spine to take up the slack. How does the disc replacement work? The disc replacement device, or implant, is designed to insert into the disc space – the gap left after the disc has been taken out – with minimal removal of normal bone or ligament tissues, and is held in place with small teeth that grab the bone, and with the normal tension of the remaining soft tissues holding it firm. The bone of the vertebrae will eventually grow directly into the top and bottom plates of the device making the fixation permanent, but right from the start the fit of the specific disc designs is such that loosening or slippage of the device is very rare, even with early motion and activity. So, they don’t need to be screwed in or cemented into place, and you don’t need to wear a hard collar or immobilizer while recovering from surgery. How are disc replacement implants designed? There have been many different designs of artificial discs created over the last 40 years, and a lot of different materials have been tried from one time or another. Spine surgeons have benefited A LOT from the much longer and sometimes fraught experience of our total joint colleagues who have been studying these issues for many decades longer. The implant designs that I use now are all FDA approved, studied in numerous scientific trials, and have been in use around the world for at least a decade in each case, and much longer in some cases. The primary design for each of the implants I use is the same: Each disc design has three parts: two metal plates – one top and one bottom - and a plastic insert or spacer in the middle. The plates are made of a mix of metals commonly used in spine and joint replacement surgery (cobalt, chromium, and molybdenum in some cases, and titanium in others). The plates typically have either teeth on the top and bottom that help hold the plates to the vertebrae, or small thin “keels” that slot into the bone above and below. The teeth or keels are pressed into the bone without any bone removal, which makes the implant designs I use easy to place properly, without cutting away normal bone. The surfaces of the top and bottom metal plates are typically sprayed with a coating of a bone forming material (hydroxyapatite) that stimulates the vertebral bone to grow and attach to the metal plates for long term stability. The plastic insert that fills the space between the plates differs from implant to implant. In most implants the insert is made from a high molecular weight polyethylene, a material with enough density to resist wear and deformation over time, but “slick” enough to provide very little friction as it slides back and forth against the upper and lower plates. This is the same strategy and material used in our most successful and long-lasting hip and knee replacements. The insert is designed to move a little back and forth and side to side as you move your neck, mimicking your natural joint motion. How big is the implant? They come in different sizes, in order to properly fit different size patients. (Interestingly, your body size does not necessarily tell me much about the size of your spinal elements: some very big people have a surprisingly small bone structure, and vice versa!). Typically, though, the implant is not much bigger than the size of your thumbnail, and not taller than two or three quarters stacked together. The four disc replacement implants I current use are all FDA approved and well-studied across the globe. Full disclosure – I have been asked to teach surgical techniques to other surgeons from time to time, and I do participate in Investigational trials for some implants ( I was a Principle Investigator for the original MobiC two-level FDA study 15 years ago, and am an investigator for Centinel Spine’s two-level Investigational Device study now), but I am not a paid consultant for any of these companies. So, I can honestly say I pick the implant that suits my patient’s situation best, each time! MobiC – ZimVie is a new name for a long-established company, and the most widely used two-level implant in the US. You can learn more about their implants here. Pro-Disc-C – One of the first to bring an artificial disc to the lumbar spine world, they have a long-established and successful product for single level surgery, and Centinel Spine is sponsoring an ongoing investigational study for their new implants for two-level surgery. M6 – Provided by Orthofix, this implant has a unique central core that also provides a little more cushion, in theory, than the solid high molecular weight polyethylene cores, and fits certain disc configurations very well. Simplify – A newer entry provided by Nuvasive, this implant has titanium plates top and bottom, which eliminates any concern for those with metal allergies, and is approved for two level use.
Thanks for reading! I hope you found this both interesting and informative. Feel free to Like and Share this content and please comment to let me know what other questions you might have!
1 Comment
Pam Huff
5/9/2023 10:14:57 pm
Good evening, I had a cervical fusion and discectomy done on 5, 6 and 7, in 2016 and recently am experiencing headaches and severe pain in neck area and top of spine, along with numbness in finger tips. I went to my primary today who prescribed Medrol dose pak, did a Toradol 60 mg injection and Flexeril 10 mg as needed. Also did PT referral along with a MRI request after PT. She requested I see an my ortho after all of the above. I prefer seeing someone from CC and saw your name on Dr Gobezie's website, who happened to do my shoulder re-construction in 2015 and I trust completely.
Reply
Leave a Reply. |
Details
AuthorI'm Dr. Rob McLain. I've been taking care of back and neck pain patients for more than 30 years. I'm a spine surgeon. But one of my most important jobs is... Archives
January 2024
Categories |





 RSS Feed
RSS Feed