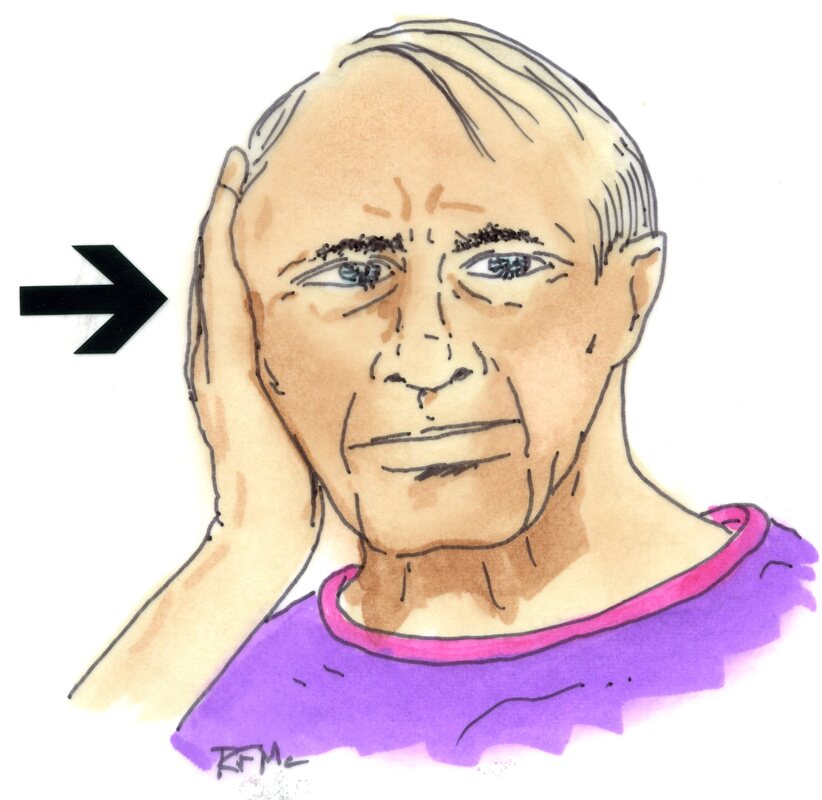
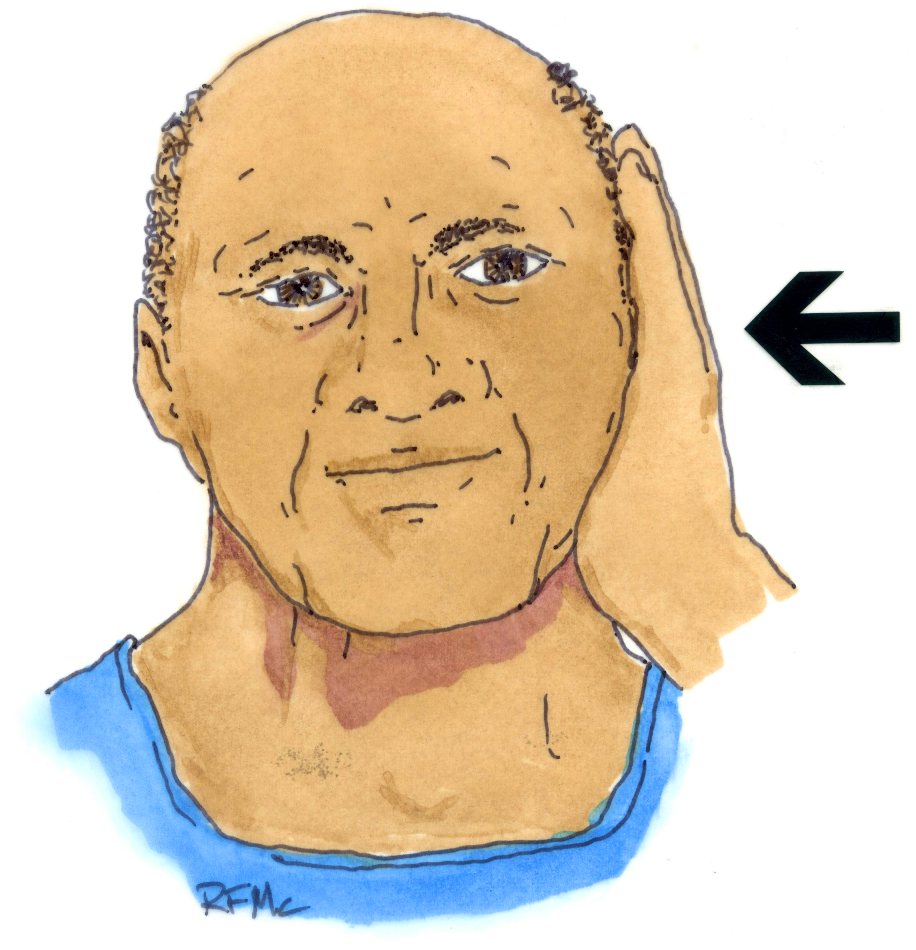
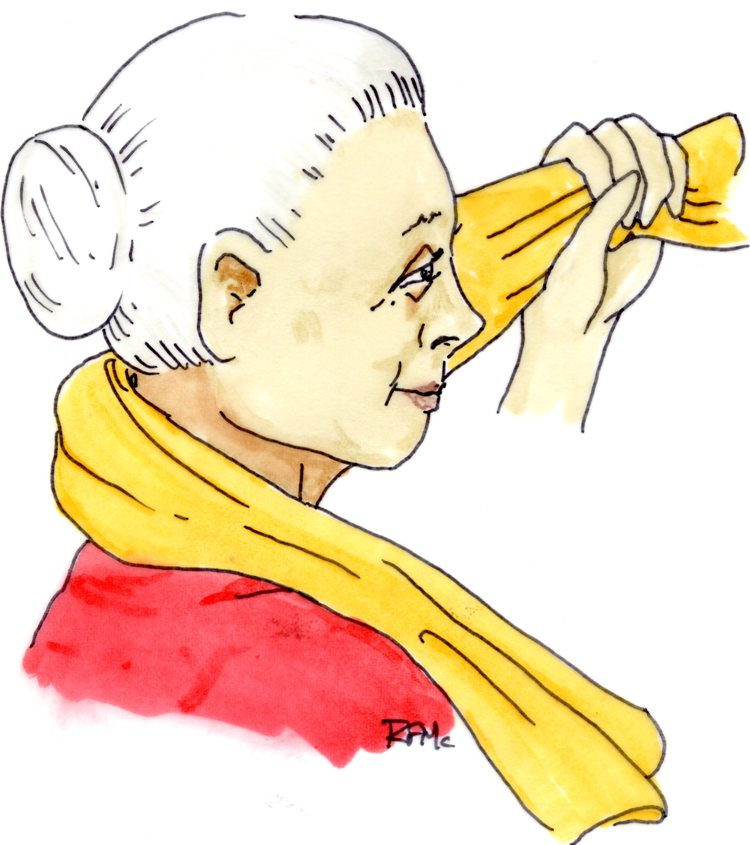
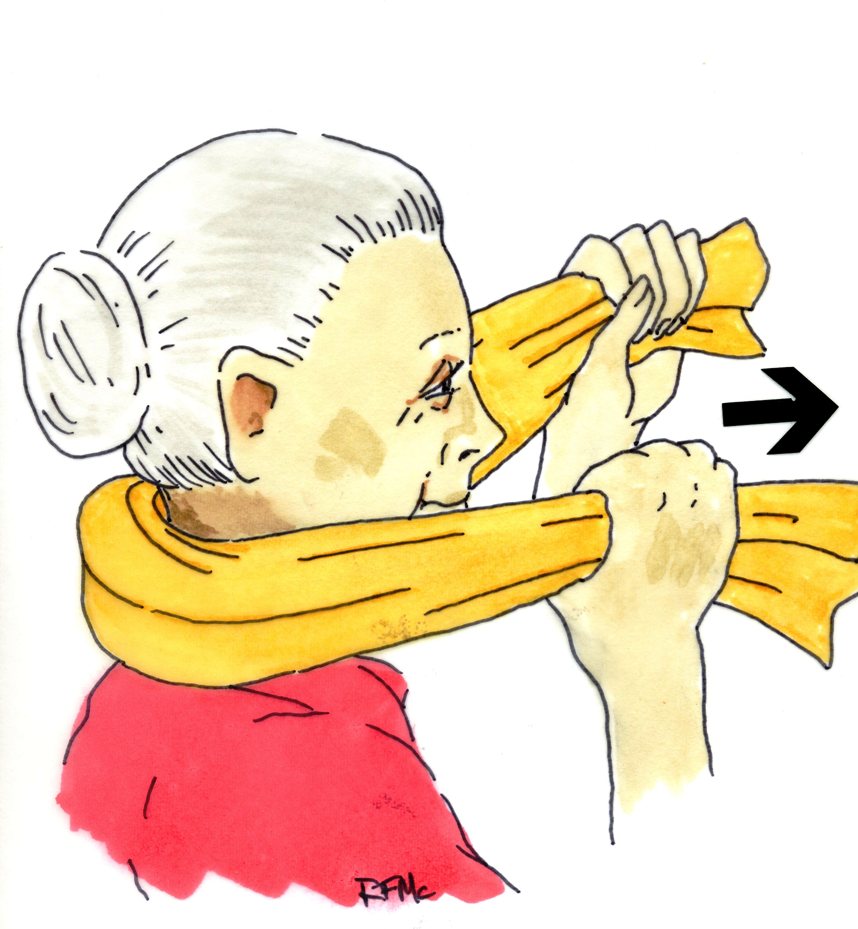
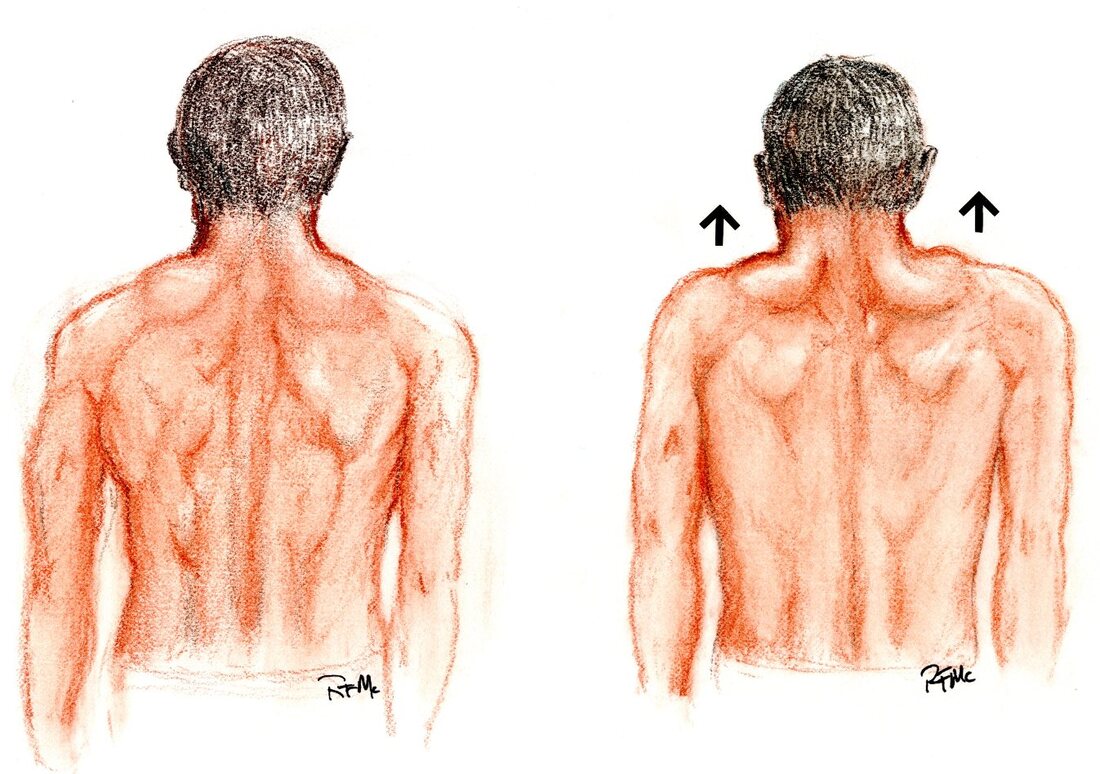
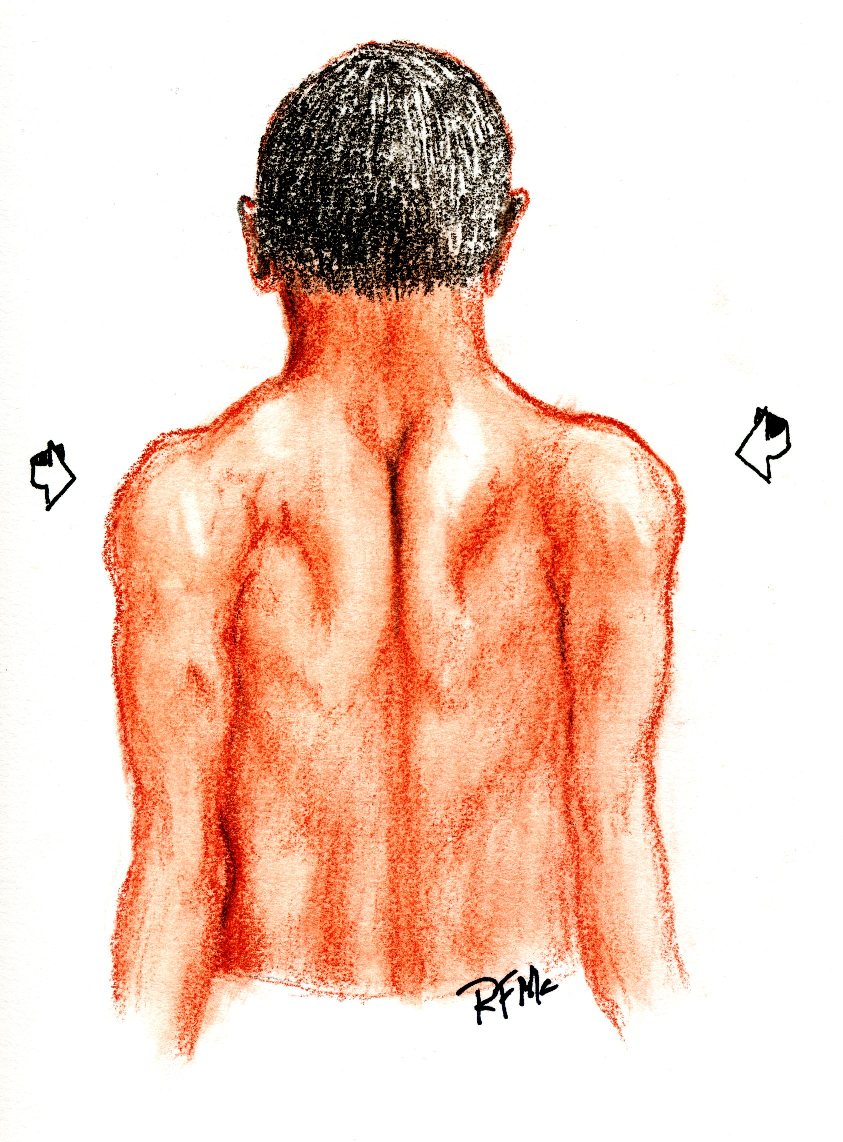
Cervical Spine Exercises for preop and post-op patients alike Any and every patient that comes through my clinic for neck pain or radiculopathy will have some need for an exercise and neck fitness program, if not to avoid cervical spine surgery then to recover from it. It’s universally recognized that an exercise program can reduce neck pain and spasm after an injury as well as surgery can, in most cases, and that after months of pain and limited activity the muscles that support our head and neck weaken and become very susceptible to repeated aggravation and reinjury. So, a good exercise program is IMPORTANT whether you are avoiding surgery or recovering from it! Stretching exercises: It’s usually not necessary to work hard on stretching the neck to regain motion. After an injury or after a bout of muscle spasm, most patients can regain range of motion by working very gently on 3 types of stretching activities: Gentle stretches: First of all, patients can start by sitting in a common kitchen chair and gently working on relaxation: letting their shoulders relax and letting their neck stretch forward, letting the chin and shoulders fall forward, and relaxing the muscles so that they ease into a slumped posture. Let this go for 10-20 seconds before sitting upright and stretching the neck back into normal position. Do this a few times until you feel a bit looser. You can then also stretch your neck backwards by laying flat on your back at the edge of the bed and letting your neck hang over the edge. By gently letting the head roll backwards, you can stretch the muscles in the front of the neck and relieve painful tension. Finally, while sitting in a chair, you can let your chin fall forward and your head flex forward as far as is comfortable, then gently roll it from side to side, trying to let your ear almost touch your shoulder as you get to each side. You can continue this rotation all the way around the back until you are looking at the ceiling. Then let the spine roll to the other ear and back around in a circle. This gentle range of motion will help stretch all the muscles; it should be done as comfortably as possible with no attempt at actually straining or causing pain. You don't need to push your comfort level. Isometric strengthening exercises: Next come the exercises to help restore strength and stamina for the muscles that support your head and neck. Start with this series of gentle isometric exercises that will help strengthen the support muscles of the neck: These exercises should be done gently to start with and are never intended to involve great strain or produce pain in the neck. If the exercises make you sore, but the soreness is gone by the next day, then you are exercising and working the muscles. If the soreness persists more than a day, however, than you may be overdoing it, and need to back off as the strain may be too much. Isometric exercises are intended for you to strengthen the muscles without motion of the head or neck. In other words when placing the hand against the side of the head and pressing against a head the hand should not push the head over, nor should the head push the hand away, but both should stay still by pushing against each other equally. This will help the muscle strengthen but won't strain the neck or require great range of motion. Side bending exercises: Start off by placing the palm of the hand against the side of your head around the level of the ear or a little higher. Press against the side of your head with the hand, not trying to twist it or bend your neck, and push back against the hand with your head. You will feel the muscles along the side of your neck and in the front of your neck tighten as you push. Count to 10 than rest and relax. Do this about 5 times to the left-hand side and then 5 times to the right-hand side and then rest and relax. This will help strengthen the muscles both in the front and the back of your neck. Forward bending exercise: Just as you used your hand to press on the side of the head, this exercise simply requires that you push against your forehead with your hand. Pushing back against the forehead as you push forward with your head you'll tighten the muscles in the front of your neck, and you can feel of those tighten along the front of your throat as you push. Do this exercise for a count of 10, resting between sets, and do about 5 sets before you quit. Extension exercises: Use a small bath towel and place it like a sling behind the back of your head, just at the base of your skull. Pull the towel up against the back of your head with both hands and pull forward firmly. Push back into the towel with your head so that you do not either bend your head forward or push the towel away. As you push back into the towel you will feel the muscles on the back of your neck and into your shoulders start to tighten and firm up. This is another exercise that you should do for about 10 seconds at a time using 5 sets as a normal set of exercises. You can do all these exercises while sitting and watching your favorite show, while sitting for lunch, or anytime you have a half-hour to yourself. Shoulder Girdle exercises: When you have done your isometric exercises for the neck muscles, you may start doing exercises for the shoulder girdle itself. When we talk about the shoulder girdle, we are talking about the muscles that attach to the neck from the shoulder blades along either side and from the middle of the back. These muscles include the trapezius muscles, the spinal muscles that run right along the spine, and muscles that support the shoulder blade, or scapula, on either side of the neck. Getting these muscles back in shape is often a turning point to overcoming upper back and neck pain and fatigue. Start by standing upright with your shoulders level and let your shoulders relax at your sides. Once you have relaxed, with your chin up and neck in neutral position, shrug your shoulders up towards your ears as far as you can, and tighten them and hold them for a count of 10 before resting, letting them come back to their normal position. You can do this exercise while holding weights in your hand, but I would start with no more than 5 pounds in the hands and work up gradually with weights if you want to. As you get comfortable with this you can add more repetitions and perform the shoulder shrugs as you rotate your shoulders – still with your arms at the sides - from front to back, ten times. A final exercise that will help build the shoulders up is to squeeze the shoulder blades together as though you were trying to pinch a piece of paper between the shoulder blades behind your back. Squeeze the shoulder blades together and hold on there for a count of 10 then rest and relax.
Hopefully these exercises will get you back to better neck motion, better activity, and restful sleep. Give any physical therapy program time to work – results can be seen after 6 – 8 weeks of exercise, but not after 6 – 8 days, so don’t get discouraged. And remember to use your anti-inflammatory medications, and ice and heat as needed, to help with soreness and stiffness. For more information on neck pain, cervical disc disease, and the surgeries that can treat them, browse for other links on my website at spinesurgerycleveland.com. I hope you found this information useful. If you did, consider liking and sharing with others. Thanks for reading!
1 Comment
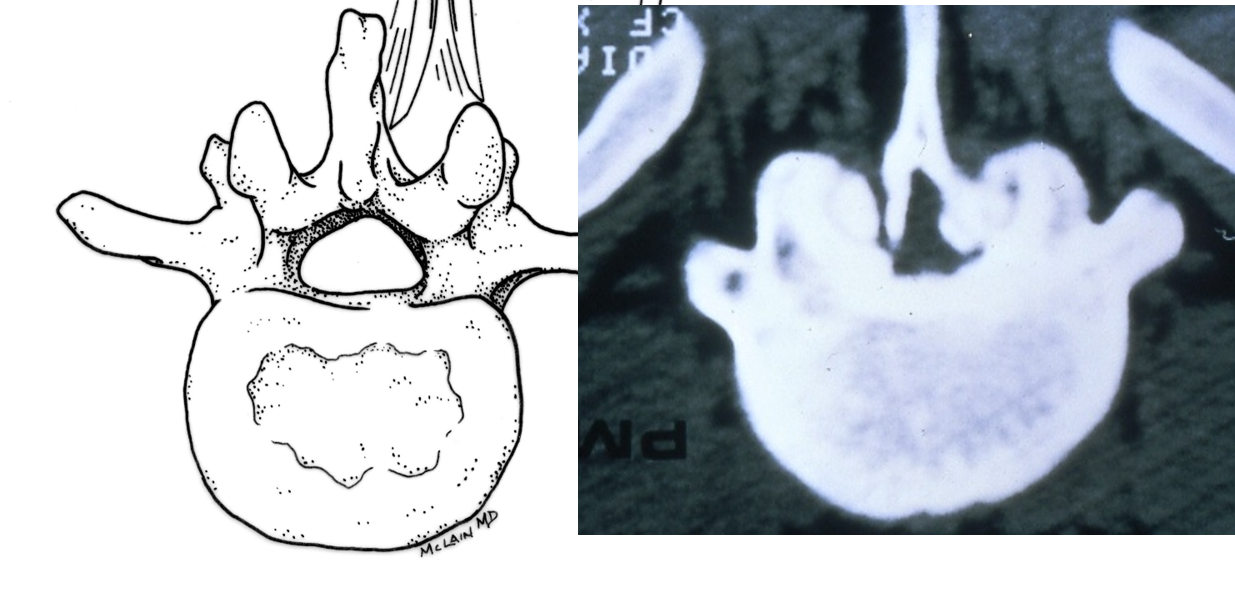
When you’re sitting down, you feel fine. A little back pain but no problems. And when you first get up, you’re ok too. But over the last year you’ve noticed that you can’t walk as far as you used to, that your legs start to tingle and feel funny if you have to stand too long in one place,and that – unless you lean on the shopping cart – you just can’t get around the market anymore. Is this what getting old feels like!?? No, this sounds more like Lumbar Spinal Stenosis, a problem that lots of older patients have to cope with. It’s common in even my most active patients from age 60 up. However, unlike old age, this is a problem that’s fixable. The symptoms of leg pain, numbness and tingling, and progressive weakness, usually brought on by walking or prolonged standing, are classic for this condition, which is caused by a progressive narrowing of the lumbar spinal canal. This narrowing is usually caused by bone spurs and disc bulges or protrusions that build up over the years, and which eventually take up so much of the spinal space that the nerves start to get “choked off”. This happens slowly so symptoms may not be appreciated early on, and often it’s not until walking and standing tolerance are severely limited that patients realize something’s wrong. Symptoms initially seem to be a problem caused by walking too much or just being on your feet too long.
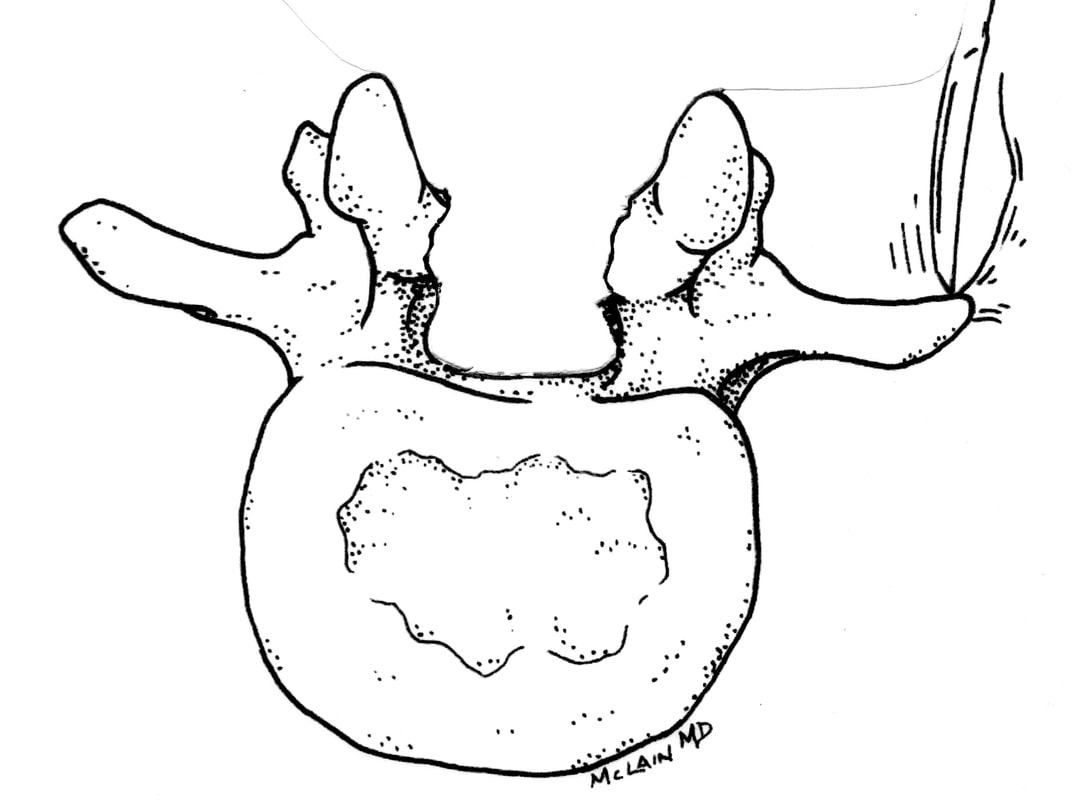
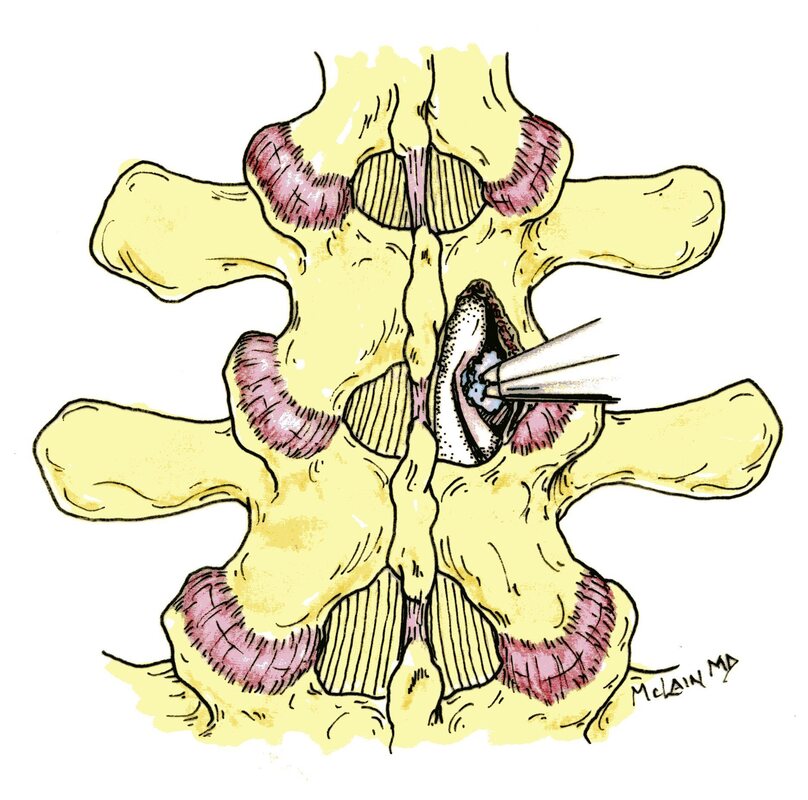
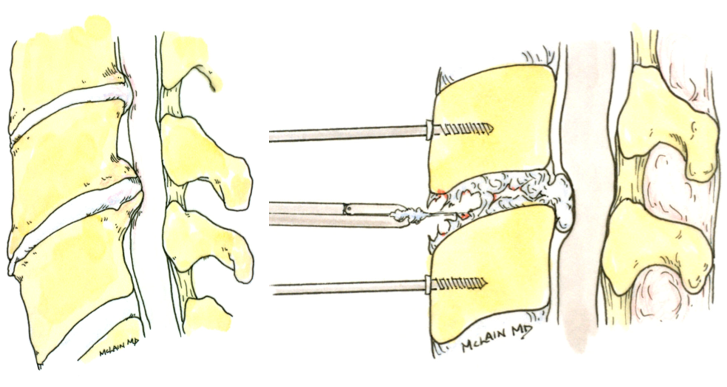
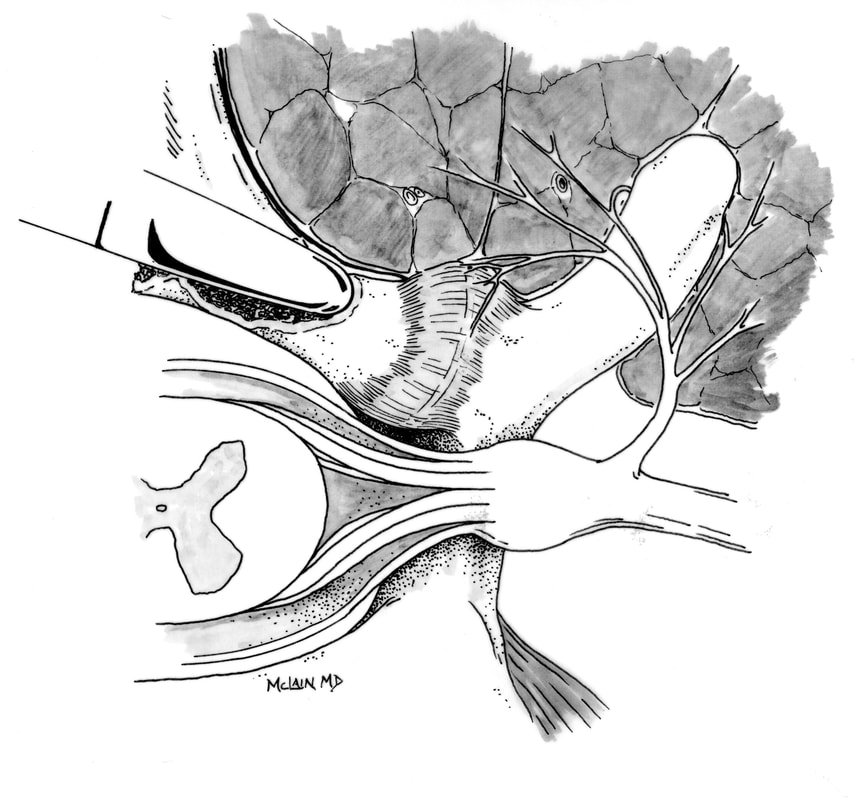
“ Doc, I feel fine when I first get going. But if I have to stand in one spot for any length of time, there comes a point where I feel like I’ve got to either sit down or fall down!” This is because the upright position of the spine when we stand, or extend our lumbar spine, takes up a little bit of the remaining room the nerves need to continue functioning. If you hold that position too long, its similar to cutting off the circulation to your foot – the legs tend to feel woody, tingling, or painful and weak. But, your limbs aren’t getting weak per se – they just aren’t getting normal input when you are in that upright position. Your muscles may start strong but they tend to fatigue very quickly. “I stay active. I still walk for exercise. I walk two miles every day. But I know a spot every 500 feet where I can sit down if I need to!” And, as the compression gets worse, the symptoms come on more quickly and normal daily activities can become very difficult. Bending forward or sitting down gives the spinal canal a little extra room and the symptoms go away. “I can ride my exercise bike for two hours, no problem, but I can’t walk to my mailbox!” If the condition is untreated, symptoms become more severe and constant and eventually no position is very comfortable, which is when my most stoic patients finally come in. Medical management, injection therapy, and PT can help, and I usually work with an expert group of pain management specialists, but once the nerve compression gets to a certain point, physically decompressing the nerves, with a laminectomy or laminotomy, is the only reliable solution. The good news? You are not doomed!! This is one of those conditions that responds very well to surgical care, which can often be provided on an outpatient basis. After surgery, most patients do benefit from a course of physical therapy and continued nonoperative back care. If you have a chiropractor or physical therapist that you like to work with, let your surgeon know so they can stay in the loop, and help you get back to your best function. For more information on spinal stenosis and the surgeries that can treat it, check out these other educational sites or browse for other links on my website at www.spinesurgerycleveland.com. What questions can I answer for you? Comment below, be sure to like and share this content if you found it helpful! Patients with neck pain often have trouble sleeping. Sometimes the issue is simple –after laying in one position for too long, their neck gets sore and they have to change positions, so they toss and turn a bit. Other times, the problem isn’t really the neck pain, it’s the burning pain or tingling running down the arm (radiculopathy), which suggests more serious nerve compression which may require a visit to the surgeon. Most often, patients just can’t find a position of comfort, their neck hurts whenever they get into a bad position, and they can’t get to sleep, much less sleep through the night. Sound familiar? It’s not a minor issue: Inability to get a good night’s sleep leads to exhaustion, exhaustion makes it hard to cope with pain, pain interferes with function, and inability to function leads to depression, anxiety, and more problems sleeping. What can we do to get a better night’s sleep without resorting to surgery? First, we need to set ourselves up for success - to adopt good sleep mechanics or “hygiene”: stick to a consistent sleep schedule, including weekends, get some good exercise each day, don’t drink coffee or caffeinated pop late in the afternoon, and get outside for at least 15 minutes every day. Also, avoid late night television and evening cocktails – even if you do get to sleep you won’t sleep as well. Second, get together a good comfortable sleeping arrangement, that works for you. The thing patients ask me about most – the best pillow for your neck. There is no universal “best pillow” for everyone (no matter what they say in the ads!). Pillows come in all shapes, sizes, styles, and materials. The best pillow for you depends on what type of neck problem you have, what type of sleeper you are, and how you tend to sleep most comfortably – are you a side-sleeper or a back sleeper? The main goal is to keep your spine in a neutral alignment and allow your muscles to relax while you are asleep. The best pillow is the one that has the proper firmness and height (loft) to help you maintain your best alignment throughout the night. Here are four important points to consider: 1. The wrong pillow is an old one, an overstuffed or worn-out one, or one that’s too flat to support you comfortably in any position. You don’t need to buy an expensive new pillow, but you need one with a firm fill, proper contour, and enough loft to hold your head in good position for hours without settling out. 2. For stomach sleepers, the pillow needs to be thinner. This is a tough position for most neck patients. For side-sleepers, the loft needs to be considerably thicker and the pillow needs to be firm enough not to flatten out while you’re resting. That means a “fluffy” or “soft” pillow may not hold you in good alignment throughout the night. There are a number of pillows that allow you to adjust the amount of filler material so you can customize the perfect firmness and support that works for you. If you are a back-sleeper, you need a pillow soft enough to let your head sink in a bit, but firm enough to support your neck. Some pillows accomplish this by sewing in a preformed divot in the center, providing a firmed roll at the edge under your neck. 3. There are a number of contoured pillows on the market, and a number of websites that “prove” the value of a specific brand, and they may advertise memory foam over latex foam. Check multiple sites to get an unbiased opinion. Most contoured pillows have special ergonomic designs that try to hold your neck in its best natural alignment. They may have a shallow center cavity to gently cradle your head, and a firmer, mounded rim for cervical support. These are pillows primarily intended for back-sleepers. 4. Some people will find that a simple roll-pillow gives them the best comfort during the night. Others may find that they do best with two pillows – one for starting out on their back, and a second one to support when they want to sleep on their side. You don’t need to buy the most expensive down-stuffed pillow you can find, but don’t skimp. The well-made designs are often available in cheaper versions, but the materials will be different and the support will be lacking. Obviously, there are no hard and fast rules, and some trial and effort is inevitable. Hopefully this will guide you in the right direction, and help you get a good night’s sleep. Thanks for reading and let me know what other questions you might have! Spine surgery has a complex and confusing language. You need to know a little of it...Patients considering spinal surgery often come to me for a second opinion, having already been told they need an operation, but not really knowing what it is they’re actually having done. Some of this is because spinal disorders are complex, and the anatomy is complex, and the procedures can be complex. That’s why you go to a spine specialist for surgical treatment. But a lot of the confusion is because the language we use is confusing, and – even though we’re spine specialists – we don’t always explain ourselves very well. One common question comes up after we’ve discussed the need for spinal decompression – surgery to take pressure off the nerves in the neck or back – and it really distills down to “What did you say??” Spinal decompression is just that – taking the pressure off of the “neural elements” (nerves or spinal cord) by removing bone and expanding the space the nerves pass through. Sometimes your surgeon may simply inform you that you need a “decompression” without explaining what that means, and the specific terminology can be important. So, ask for more information. They may tell you you need a Laminectomy. A laminectomy is a type of decompression that involves removing the bone that forms the roof of the spinal canal, allowing the surgeon to remove bone spurs or disc herniations that may be pinching the nerves in the canal. This is the widest decompression your surgeon can do, and it’s often necessary for patients with spinal stenosis or those needing a fusion as well. Or maybe they mentioned a Hemilaminectomy? That’s just a partial laminectomy, performed on one side of the spinal column. Or a Laminotomy? Or a Hemilaminotomy? Those are essentially the same thing - smaller windows still, removing just enough bone around the point of pressure to allow removal of the disc or cyst or spur that’s causing the pain. Microdiscectomy? That just means your surgeon is going to use magnification while operating through a small incision and remove a herniated disc through a hemilaminotomy, to take pressure off the nerve with the least injury to the surrounding tissues as possible. When cord or nerve compression occurs in the cervical spine, it is common to perform an anterior cervical discectomy and fusion, or ACDF. In this case the decompression is through the front of the neck, removing the entire disc from between two vertebrae, then stabilizing the spine with either a fusion or an artificial disc. This allows us to take the pressure off the spinal cord and nerve roots without having to move or manipulate the very sensitive cord from behind.
So, if you’ve been told you need a decompression, just ask for more information – what kind and where? Your surgeon should be happy to give you a description of what their plan is. And if you want some good illustrations of exactly what we’re talking about, check out some of the other pages on my website, www.spinesurgerycleveland.com for links to some excellent and reliable resources! Thanks for reading. Got any questions? Comment to let me know... 9/11/2022 Cervical disc disease: My hand and arm are going numb and my Doctor thinks it’s my neck…does that make sense?Read NowMy hand is numb, tingly, and I’m dropping things!It’s pretty common for neck problems to cause symptoms in the shoulder, arm or even down to the hand and fingers. Any changes in your cervical spine that irritate or compress a nerve can cause symptoms in the part of the arm that nerve goes to. That’s called radiculopathy. Neck pain and arm pain are really two sides of the same coin. And depending on your “coin”, you may have neck pain, arm pain, or both. The wear and tear changes of daily life can cause the cervical disc to break down, bulge, or herniate. When the disc degenerates, it loses its ability to be a good shock absorber and support and stabilize the vertebrae that make up the spine. The disc may rupture or may just bulge into the canal and harden. The arthritic disc can cause neck pain, muscle spasm, stiffness, and headaches. On the other side of the coin, that bulging or herniated disc may press directly on one of the nerves leaving the spinal canal and going into the arm. Worse, a large disc protrusion may press directly onto the spinal cord itself. Even if the disc doesn’t physically compress the nerve, it can irritate it, or it can generate bone spurs that can “pinch” the nerve even years after a recognized injury. When the nerve is irritated or compressed, we get radiculopathy: pain running down the arm in the pattern of that particular nerve. That pain may be severe and electric, may be accompanied by numbness or tingling (usually a very unpleasant numbness and tingling) or actual weakness. Neck pain can be severe and limit activity, but it’s often that arm pain that drives the patient to the doctor, because it can be intense! If you’ve got pain in your knuckles, or a sharp pain in your wrist, is that radiculopathy? Probably not. Radicular pain affects the whole distribution of the pinched nerve, and pain or symptoms run down the length of your arm as far as that nerve goes. It’s like an electrical circuit: When one light in the room goes out it’s probably the bulb. When all the lights go out – you’ve blown a fuse! So, pain running down your arm to your numb, tingly hand – that’s most likely radiculopathy and it’s probably coming from a herniated disc or arthritis in your neck. Your doctor will want to:
And that is where I can come in. Thanks Again! Not-so-obvious signs you’ve got a Neck ProblemIf you’ve woken up with a painful stiff neck after a hard day’s work or a slip and fall, you know it’s not hard to figure out where the problem is coming from. Fortunately, most episodes of acute neck pain are muscle-related and will get better with time, stretching, and some anti-inflammatory medications. You’ll usually be feeling better before you can even get around to seeing a specialist. Symptoms of more serious cervical disease may not be so obvious: Here are five symptoms you might not even recognize as coming from your’ neck, that suggest you may need to see a spine doctor sooner rather than later! 1 Numbness and tingling in the hand or arm – often confused with carpal tunnel syndrome. Numbness, tingling or weakness in one hand or the other may be caused by a nerve being pinched in the arm or in the neck. Sometimes misdiagnosed as neuropathy, if symptoms occurs in one arm and not the other, and if they persist or progress, this needs to be checked out!
2 Frequent headaches – usually at the end of a long day, and localized to the base or back of the skull. Headaches are very common, usually benign, and not given much consideration unless they become frequent or are associated with other neurological problems. Muscular tension caused by cervical disc disease can be a cause of recurrent headaches as well as neck pain. 3 Pain in the thoracic spine – right down between the shoulder blades. This often confuses patients and doctors alike, because the pain and tenderness are focal to the thoracic spine, between the shoulder blades. This is where the muscles that support your neck (the shoulder girdle) tie in to the spine, and this is often a spot where neck muscle irritation or strain is felt. 4 Loss of balance and difficulty walking a straight line – “I walk like a drunken sailor”. When we lose our fine sensory feed-back from feet and hands, we lose our sense of where our feet are in space. Without that fine neural feed-back we tend to stagger about, particularly in the dark when we don’t have our normal visual cues to help us navigate. This is called ataxia, and it’s often the first noticeable symptom of spinal cord compression. 5 Difficulty buttoning buttons – loss of manual dexterity. Even before numbness or pain becomes noticeable, some patients see a change in their hand-writing or their manual dexterity. In one Japanese grading scale of spinal cord function, patients are graded by skill using chop-sticks. If you’ve been using chop sticks all your life, and you suddenly start having trouble handling them – you need to find out what the problem is. It could be arthritis in the hands, and it could be carpal tunnel syndrome, but if it’s not one of those it’s time to examine the cervical spine. The same goes for handwriting and normal daily activities. Fortunately, the question of whether your neck plays a role in these symptoms can usually be settled with a directed physical exam and a set of plain x-rays, things your family doctor or physician’s assistant can accomplish easily. If there’s still concern after that, an MRI will most often establish the diagnosis and tell us whether this is something that can be managed simply, or whether there needs to be a discussion about surgery. And, that’s where I come in! Thanks |
Details
AuthorI'm Dr. Rob McLain. I've been taking care of back and neck pain patients for more than 30 years. I'm a spine surgeon. But one of my most important jobs is... Archives
January 2024
Categories |





 RSS Feed
RSS Feed