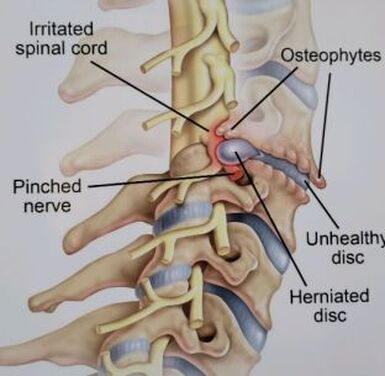
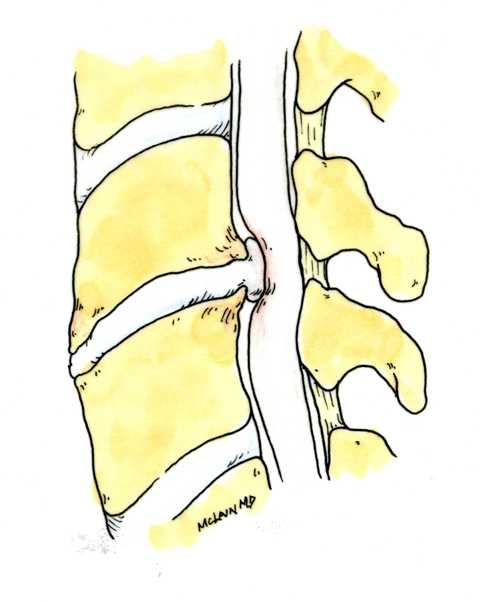
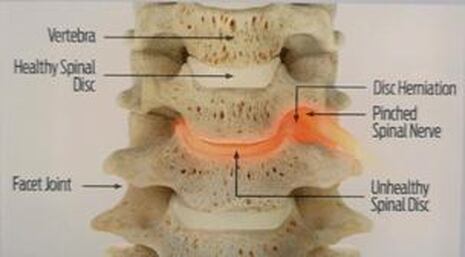
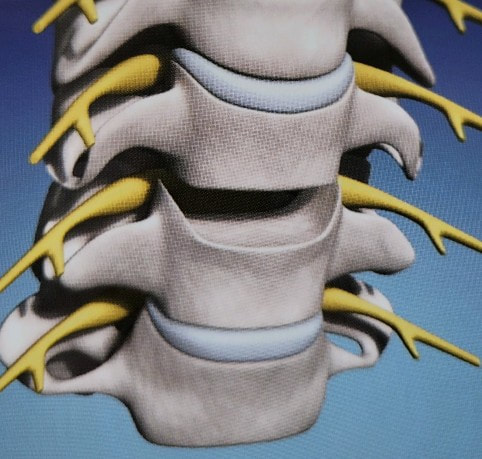
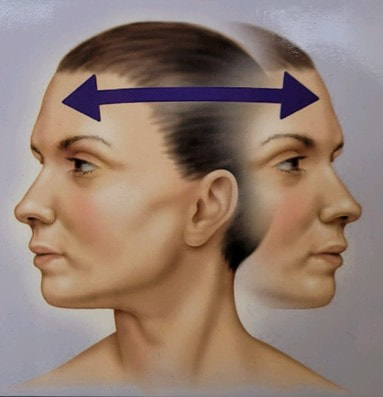
Disc replacement surgery is growing in popularity, but there is still a lot of misinformation out there, and it’s still hard to figure out which facts are FACTS!Cervical disc replacement - or disc arthroplasty - represents a powerful, well-established tool for treating herniated discs and degenerative disc disease in patients who have persistent pain and impaired function due to neck and arm pain, and who want to avoid a spine fusion if they can. So, what’s the role of Disc Replacement Surgery in 2023? There’s more good news and no bad news… Good news!! Most patients with neck pain can recover without surgery: 80-90% will get better, and get back to normal activity with physical therapy, anti-inflammatory meds, rest, activity modifications, chiropractic manipulation…or, in some cases with nothing but time and TLC! For the 10-15% of patients with a serious neck problem that just doesn't respond to time and supportive therapy, many will need an operation. Many of these patients will need a discectomy - a removal of the cervical disc through the front of the neck - to relieve the neck pain and spasm, and the persistent arm pain, numbness, and weakness caused when a spinal nerve root is compressed by a degenerated or herniated cervical disc. This is not a minor surgery, and rarely the first choice in a patient's care, but when pain is bad enough that it interferes with daily function, employment, fitness, and/or sleep…surgery starts to make sense. Who needs spine surgery? We consider surgery the first choice for patients who have more serious issues such as fracture, infection, or tumor. These conditions are relatively rare, often emergencies, and not the sort of thing we usually see in patients with persistent and long-standing neck pain problems. More commonly we are considering surgery for patients with wear and tear and degenerative neck pain problems, or those with a disc herniation related to repetitive trauma or a sudden accident. While we think of surgery as the ultimate treatment for neck pain that won't respond to anything else, we know that surgery is the most reliable solution for most causes of arm pain or weakness (radiculopathy) including disc herniation, cervical stenosis, or spinal instability. Not every type of operation works for every type of spine problems, though, and while disc replacement surgery is an excellent treatment for disc herniations and disc degeneration, it is not a treatment for spinal instability or deformity, and not at all useful for treating tumors, infections, or fractures and dislocations of the cervical spine. Cervical fusion remains the very best solution for each of those problems. For those patients who do suffer neck and arm pain due to disc degeneration or herniation, though, disc replacement – or cervical arthroplasty – is an important option. What is disc replacement surgery? Disc replacement surgery and disc arthroplasty surgery are the same thing. Also referred to as an “artificial disc” the implants used in these surgeries are designed to preserve motion in the spine after a discectomy (removal of the disc) and they have been shown to maintain motion and reduce the likelihood of degeneration at adjacent levels of the spine, something that often occurs in the years following a fusion. They are recommended for patients aged 18 – 70 years, but I, and other surgeons, have had excellent success in selected patients over the age of seventy years. Artificial discs are placed in the neck through the front of the spine (an anterior approach) after a damaged disc has been surgically removed to treat neck pain associated with radicular pain – the arm pain caused by a “pinched” nerve. In the neck, this is exactly the same approach we use for most disc surgeries and all anterior cervical fusions. Disc arthroplasty implants are not experimental or untested. The implants we have now have been in development for over 40 years and similar designs have been available for patient care for nearly 2 decades. There are disc replacement implants specifically designed for the cervical spine (neck) and for the lumbar spine (lower back). They are specifically intended for treatment of degenerated or herniated discs in otherwise healthy patients. There are no discs designed for the thoracic spine, and they are not intended to treat fractures, infections, scoliosis, or spondylolisthesis. And, to answer a pretty common question - you can’t undo an old fusion and put in an artificial disc later! Artificial disc replacement can be carried out as an outpatient surgery, and utilizes many minimally invasive techniques, but it is not “minor surgery”. When it comes to the spine, there is no such thing! The importance of surgeon experience and skill is reflected in the careful diagnosis and plan for treatment, and the skillful approach and placement of the implant. Surgeon experience with disc replacement procedures is important to the outcome here. Ask your doctor what their experience level is and whether they've treated cases like yours before. Disc replacements last a long time. How long? We don’t really know, because – unlike artificial hips and knees – we haven’t seen any of the ones we use today wear out. We have had the opportunity to observe patients from Europe who have had disc implants in place for up to 35 years without failures. As an investigator for early trials of two-level disc replacements, I have followed my own patients for more than 18 years without seeing any cases where the disc has worn out or deteriorated. Who needs disc surgery? Disc degeneration is a process that occurs over time, with wear and tear, age, and physical and environmental stress that causes changes in disc that separates each of the vertebral bodies in our spinal column. Each disc acts as a shock absorber and a slightly flexible joint that allows the spine to move, but only so much. As we age, the molecular components of the disc change, resulting in a loss of water content. The disc loses height, becomes tougher and harder, and becomes a less successful shock-absorber. As this happens, the disc may bulge or protrude into the canal where it can press on the spinal cord or nerve roots, causing arm pain, and it can lose its ability to control neck motion or cushion the small joints during motion, resulting in neck pain As these changes progress we see: Axial neck pain – pain in the joints, muscles, and ligaments of the neck, causing focal pain and stiffness; Referred pain - symptoms over the shoulder girdle muscles that support the neck - the trapezius, rhomboids, and paraspinous muscles and Radicular pain - pain running down the arm and into the hand and fingers in a pattern or distribution typical of a specific nerve level, caused by pressure on the spinal nerve at that level. Radicular arm pain can be uniquely intense and is the symptom that drives most patients to ask for surgery. When these symptoms fail to improve after a trial of non-operative care, that’s when we consider surgery. We generally consider surgery for patients with:
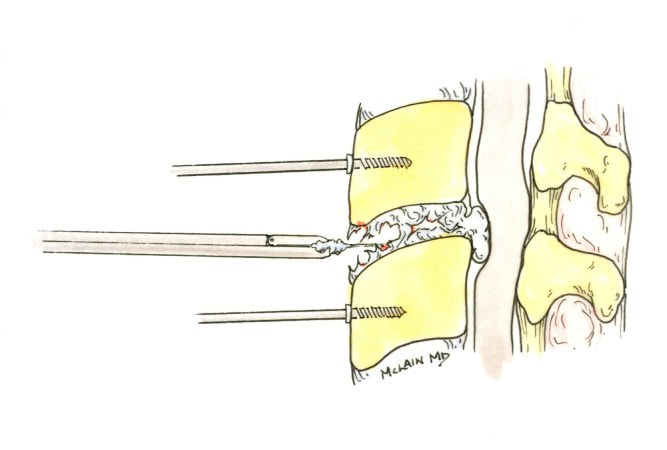
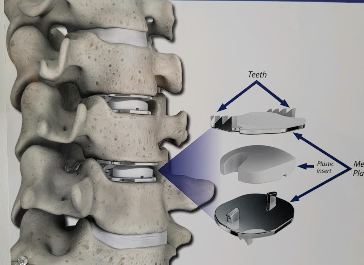
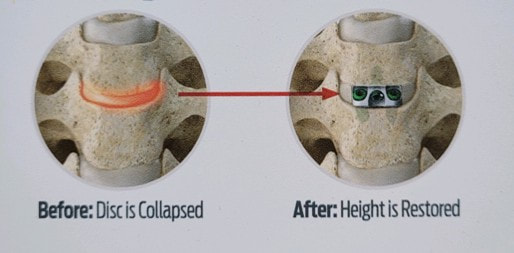
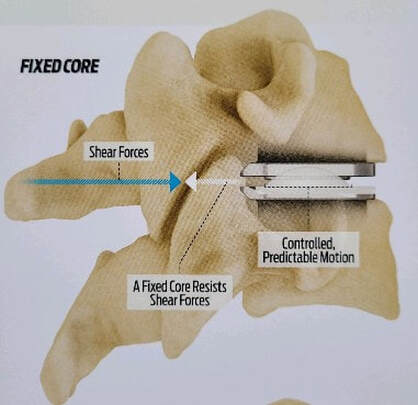
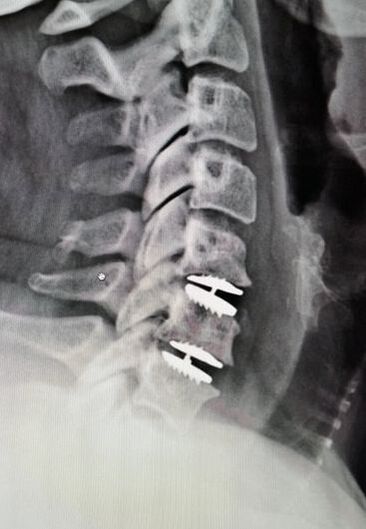
The traditional treatment for cervical disc herniation has been fusion, typically described as an "anterior cervical discectomy and fusion" (ACDF). That’s a surgery through the front of the neck, with complete removal of the disc back to the spinal canal and removal of disc or bone spurs that may be pressing on the nerves. But, why fuse the spine after we get the disc out? The interbody fusion is performed by placing a cage or bone spacer between the endplates of the adjacent vertebrae to restore the intervertebral and foraminal height, immobilize the painful segment, and provide permanent stability. Fusion does all of these things reliably and well! But fusion eliminates motion at the treated level and increases stresses in the adjacent levels above or below, and that can lead to breakdown at that adjacent level, (adjacent level degeneration) sometimes just a year or two after the initial surgery. What does the Artificial Disc do that’s different? The cervical disc arthroplasty or disc replacement is intended for the patient who: - needs the discectomy and would otherwise need a fusion, but - still has motion at the injured level and wants to avoid the down-time required for a cervical fusion to heal, - wants to avoid the risk of non-union (fusion failure) that might require another surgery, and - wants to avoid the risk of adjacent level disease down the road. The approach for the disc arthroplasty, and the removal of the damaged or herniated disc during disc replacement surgery is exactly the same as in the ACDF, but instead of placing the bone or a fusion cage in the empty disc space, disc replacement surgery fills the space with an artificial device that restores disc height and alignment and preserves the motion of the original disc. This allows the treated spinal level to move more naturally, reducing the risk of adjacent level degeneration down the road. And there is no need for prolonged immobilization or restricted activity, as we don't need to "wait for fusion". Who is the best candidate for a disc replacement surgery?
Where will disc arthroplasty work well? Success has been unequivocally demonstrated in the well-maintained but painful disc, in the young and active patients. There are over 150 peer-reviewed publications analyzing investigational FDA trials, long-term follow-up studies, and large multicenter studies to ensure the safety and effectiveness of these implants. These studies have shown that, when used for the correct indications in the properly selected patients, disc arthroplasty provides significant advantages over traditional fusion procedures. They are not "experimental or investigational", and their effectiveness is proven. Do they work in everyone? As we noted at the top of the page, these implants are not intended to treat problems like infections, tumors, or fractures, and they can't undo what has already been done. But they can be considered in almost every patient who would be a candidate for a one or two-level ACDF, so long as the patient has good bone quality and still has motion left at the level to be treated Severe osteoporosis makes any sort of stabilization difficult, and disc replacement is as likely to fail as a simple fusion, but would require a more complex revision that a failing fusion might. And, a patient with no remaining motion at an arthritic level has already started to fuse naturally, and is unlikely to get good motion back with any operation. The disc arthroplasty is a motion-preserving procedure, but it can't undo a solid fusion. What about age? If patients are reasonably fit and bone quality is good, age isn’t a big problem! Large studies and FDA trials of disc replacement have included patients up to age 69, and my experience with patients older than this suggests disc replacements are actually better tolerated than the traditional fusion. At age eighty, some of my fit patients do very well with outpatient disc replacement surgery, returning home within a few hours of their operation, with a soft collar, and no restrictions of daily activity. There has to be good bone quality and good residual disc motion, however. What about activity level? Patients who are athletic or hard working can depend on disc replacements to hold up to their physical demands – the discs are not fragile and the patients don't need to feel fragile either. Patients don't have to restrict their fitness or work activities beyond what makes sense for normal people. What about smokers? Well , first off – stop ! It’s not good for you. However, smoking does not affect the fixation of the disc replacement implant the way it can impede bone formation needed for fusion. Studies to date have not shown smokers to have any poorer outcome after disc replacement surgery than nonsmokers. That's just not the case with fusion, so disc replacement is probably a better choice for you too. With all that in mind, cervical disc arthroplasty continues to offer an attractive and valuable option for most patients otherwise indicated for cervical fusion to treat their neck and arm pain. If you’ve been offered a fusion surgery, ask your surgeon if you’re a candidate for disc replacement! As always, I hope you find this discussion interesting and useful. If you have other questions that I can answer for you, please comment below. If you want more updates on blog posts please like and follow me on my Facebook page.
And feel free to like and share this content with others that might find it beneficial! Thanks for reading.
0 Comments
Leave a Reply. |
Details
AuthorI'm Dr. Rob McLain. I've been taking care of back and neck pain patients for more than 30 years. I'm a spine surgeon. But one of my most important jobs is... Archives
January 2024
Categories |











 RSS Feed
RSS Feed