|
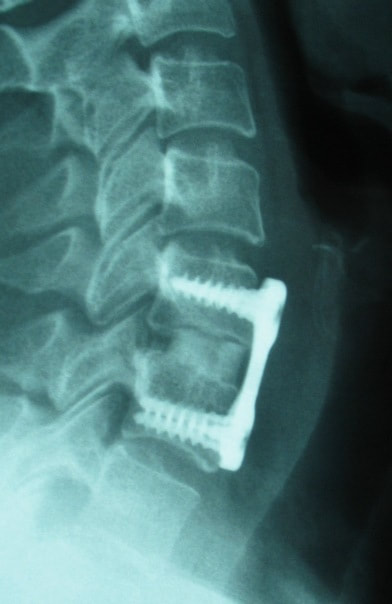
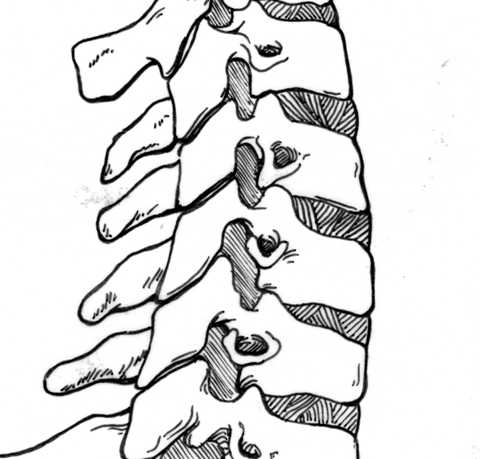
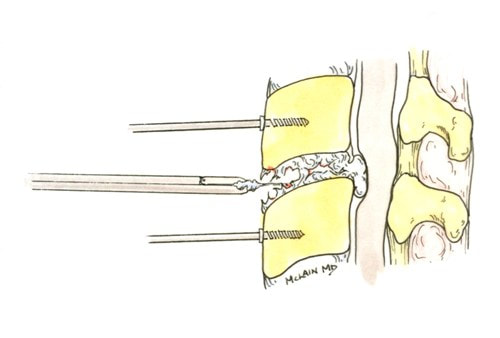
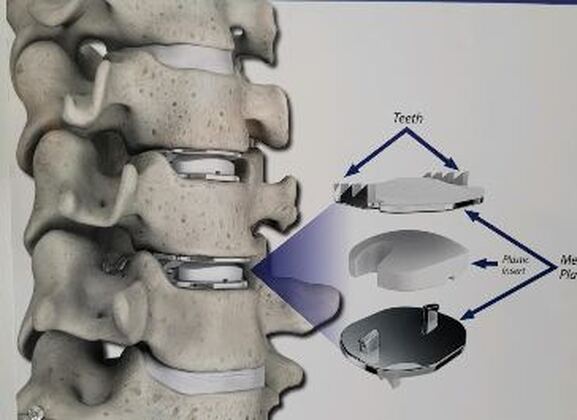
2/19/2023 Disc Replacement is an Excellent Solution for Adjacent Level Disc Disease: Five Things to KnowRead NowOne of the most concerned groups of patients I see are those who've had a previous cervical fusion - sometimes quite recently -who have now developed new neck pain or a new disc herniation at the level above or level below their fusion. This is called Adjacent Segment or Adjacent Level Degeneration, and it is a well known and common complication of cervical fusion surgery. And, until recently, it has almost always been treated with another fusion. That treatment strategy was the only one available up until ten or fifteen years ago, and it would, as you might guess, tended to start a vicious cycle of fusion and adjacent level herniation that often lead to multiple surgeries and multilevel fusions in many other wise fit and active patients. Even today there are many spine surgeons who will advise their patients in this situation that there is nothing for it, they're going to need another fusion. I've treated enough patients over the years to know that an active, young patient with a 4-level fusion is not often happy with their result. Neck pain is constant, stiffness and limitations in motion are inevitable, and there is always the likelihood that any level that's still mobile is going to degenerate, become painful and require another round of surgery. Again, up until ten or fifteen years ago there really wasn't much else that could be done. That vicious cycle was one reason surgeons and non-surgeons alike would advise their patients to avoid surgery until they just couldn't take it anymore. That approach to neck pain and disc disease is changing, largely due to the advent of disc replacement surgery as an alternative to fusion. Disc replacement surgery is growing in popularity, both because of the interest of patients, but also because of the growing number of surgeons who have been trained in these surgical techniques and who have become familiar with the vast experience of other surgeons who have preformed large clinical trials and extensive peer-reviewed studies to document the advantages and safety of the devices we now have available to us. However, there is still a lot of misinformation out there, and it’s sometimes hard to figure out what facts are important to your individual condition! And that's particularly true when it comes to patients who have an adjacent level disc herniation or degeneration adjacent to a previous fusion. Here are five points that are particularly important for these patients and their care-givers to know: 1. Disc replacement surgery (also called disc arthroplasty) has been available for roughly two decades now, and has an extensive background of supportive research and surgical experience. Use of an “artificial disc” to preserve motion in the spine after a discectomy (removal of the disc) has been shown to maintain motion and reduce the likelihood of degeneration at adjacent levels of the spine, which often occurs in the years following a fusion surgery. Disc replacements have been widely studied in a number of controlled, FDA approved trials, and have proven safety and effectiveness in all of those studies. For those studies, the patients included were very specifically selected, however. Disc replacements were recommended for patients aged 18 – 70 years, typically, but were not allowed for any older patients, patients with other illnesses, and - importantly - patient who had had a previous cervical fusion. It wasn't that they were not expected to work for those patients. Instead, it was known that including patients with too many variables in their background would make the analysis of all of data much more difficult, and could confuse the study. Comparing patients who had had a previous neck surgery to patients who had had no previous surgery would have made these early studies impossibly complicated and could have made it impossible to reasonably document their safety and efficacy for any patient. 2. Artificial discs are placed in the neck using exactly the same surgical technique used for anterior discectomy and fusion surgery, the commonly recommended treatment for adjacent level disease. The surgical approach is through the front of the neck (an anterior approach), and the damaged disc above or below the previous fusion is surgically removed to treat neck pain and the associated radicular pain – the arm pain caused by a “pinched” nerve - in exactly the same way whether a fusion is planned or a disc replacement performed. In the neck, this is the same approach we use for most disc surgeries, but it has to be carried out with added care when a previous surgery has created scarring in the vicinity. That said, there is no greater difficulty with this approach when an arthroplasty is planned than for fusion. In fact, revision surgery for fusion often requires removal of the old plate and screws before the next level can be fused, while this is not usually necessary for an arthroplasty operation. 3. Disc arthroplasty implants have been in development for over 40 years and have been available for patient care for nearly 2 decades. The implants now most widely used have been developed for placement with the most simple techniques and don't require complex surgical techniques such as placing fixation screws or fins, or cutting slots into the bone. In fact, disc replacement is generally focused on the goal of minimal bone removal and minimal soft tissue exposure, which often allows a disc to be placed successfully without ever exposing the fused level above or below. These are implants specifically designed for the cervical spine (neck) and they have very specific applications – treatment of degenerated or herniated discs in otherwise healthy patients. There are no discs designed for the thoracic spine, and they are not intended to treat fractures, infections, scoliosis, or spondylolisthesis. And you can’t undo an old fusion and put in an artificial disc later! But these discs treat the adjacent level cervical discs just as well as they do the primary disc herniations included in those original studies. 4. Artificial disc replacement can be carried out as an outpatient surgery, and utilizes many minimally invasive techniques. So, even in cases where previous surgery has created a scar or affected other levels, disc arthroplasty can still be carried out without the extensive surgery needed to remove and replace a fusion plate with a longer plate, for instance, or move the delicate tissues away from the old fusion bed to get previous hardware out of the way! The importance of surgeon experience and skill is reflected in the ability to recognize the ability to preserve motion at the adjacent level and carry out the motion preserving surgery with the minimum of soft tissue dissection and injury. Your surgeon will provide a careful diagnosis and plan for treatment, and provide the skillful approach and placement of the arthroplasty implant that allows a rapid recovery from surgery and rapid return to function. Surgeon experience with disc replacement procedures is important to the outcome in these revision operations. And, it's ok to ask your surgeon what his or her own experience has been like. 5. Disc replacements last a long time and protect those adjacent levels for a long time as well. With most contemporary arthroplasty implants we use we don’t really know how long they will last, because – unlike artificial hips and knees – we haven’t seen any of the ones we use today wear out. Most patients know either from their own experience or from what they've seen grandparents or family members go through, that hip and knee replacements tend to wear out after 10 - 15 years, and often need to be revised. With disc replacements, we have had the opportunity to observe patients in Europe who have had disc implants in place for 35 years, and we still have not seen any failures. Some of the early designs did not do as well, but those aren't in use any more and have not been for years. In my own experience I have not seen disc replacement fail or require revision. And I have followed my own patients for more than 18 years without seeing any cases where the disc I implanted has worn out or deteriorated. Is this opinion or is this fact? It is important to know that there have been over 150 peer-reviewed publications documenting the results of long-term trials and studies of total disc replacements, both here in the US and abroad. Including investigational FDA trials, long-term follow-up studies, and large multicenter studies to ensure the safety and effectiveness of these implants, almost all of these papers speak to results for primary patients and not those treated for adjacent level disc disease. These studies have shown that, when used for the correct indications in the right patients, disc arthroplasty can provide significant advantages over traditional fusion procedures. Cervical Disc arthroplasty is not experimental or investigational, and the effectiveness of disc replacement is proven. So, is there evidence that the same results can be expected for patients needing treatment for adjacent level degeneration? Is there good evidence that disc replacement can be carried out in a revision surgery as safely and effectively as it can for a primary procedure, or - more to the point - as safely and effectively as for a patient receiving fusion for that revision procedure? There is that evidence, as well as numerous series and smaller reports establishing the suitability of motion preservation for these patients who've already lost a considerable amount of their normal motion due to their first fusion. As an academic surgeon, one of my responsibilities over the years has been to track and document the results of my own patients, to identify problems before others encounter them and to establish the benefits and success of other techniques that other surgeons might subsequently take advantage of. This has also included biomechanical and anatomical studies of surgical technique and implant design, but follow-up of individual patients has always been crucial to good surgical care and the improvement of every kind of treatment. In my most recent analysis of outcomes in patients treated both for primary disc disease and those with disc herniation or degeneration following an older fusion, we were able establish strong support for the clinical opinions discussed above: Comparing adult patients receiving one or two level cervical disc replacements for radiculopathy and/or axial neck pain who had no previous surgery to patients treated the same way, who had adjacent level spondylosis or cervical fusion, and comparing all of them to a series of similar patients treated with fusion for similar degrees of neck pain and radiculopathy we found that: Patients undergoing a primary cervical disc replacement reported excellent satisfaction and pain relief 2 years down the road - 76% percent reported minimal neck pain even with activity, and 36% reported no neck pain at all. 86% reported little or no arm pain at that point, of which 59% reported no arm pain symptoms at all. Compared to this, the patients who had disc replacement for adjacent level degeneration did as well or better - 88% percent reported minimal neck pain with activity, of whom 50% reported no neck pain at all, and 100% reported little or no arm pain at 2 years, of which 75% reported no arm pain symptoms at all! Compared to patients having cervical fusion - well, they did well also, but as early as 3-4 years after surgery 18% were reporting moderate to severe neck pain, and a few were experiencing moderate arm pain. I was pleased to present the preliminary report of this peer-reviewed material at the MidAmerican and the Western Orthopaedic Association Annual Meetings in 2022. While these numbers are too small to prove anything, they certainly support the use of a disc replacement device in patients who've already lost some neck motion, as opposed to forcing them to undergo additional fusions. And what about the safety? In our analysis of these patients - none of the patients in any group suffered a complication either during or after surgery, and none of the patients treated for adjacent level degeneration has required any other surgery. Any neck operation requires superior care and technique to get a good result without complications. None of these procedures should be considered minor surgery, even when they can be performed as outpatient operations.
So, if you’ve been told you need to have a neck fusion, for a primary disc herniation or disc degeneration or for a problem that has arisen following a previous fusion, it’s ok to ask “is there another way - a better way - to treat this?”. It's worth getting a second opinion to see if disc arthroplasty might be that better way for you! I hope you found this informative and interesting! You can learn more about disc replacement surgery, and other types of spine surgery and treatment, by checking out more sections of this website, and you can follow me on Linkedin or Facebook to learn about new updates and post that may help you take care of your back and neck. Thanks for reading!
1 Comment
10/12/2023 01:19:03 pm
Wow, I never knew that you should consider having your neck checked by a surgeon if you are experiencing constant bouts of neck pain. I wanted to learn more about neck pain after seeing a lot of this term in a novel that I read last weekend. I will be sure to follow your advice and find a spinal surgeon if I need it someday.
Reply
Leave a Reply. |
Details
AuthorI'm Dr. Rob McLain. I've been taking care of back and neck pain patients for more than 30 years. I'm a spine surgeon. But one of my most important jobs is... Archives
January 2024
Categories |










 RSS Feed
RSS Feed